Menu (linked Index)
Cataract Surgery : From Darkness, Light
Last Update: February 9, 2025
- Introduction
- What are Cataracts?
- Couching for Cataracts
- History of Cataract Surgical Procedures
- Characteristics of a Modern Cataract Surgery
- Pre-Cataract Surgery Homework
- A Modern Cataract Procedure
- Conclusion
Also refer to my post: Understand Your Eyes where you can link to other eye and optics related posts, including
Introduction
The Diagnosis
Around 5 years ago, during my routine yearly eye checkup, the optometrist casually and nonchalantly mentioned that I had developing cataracts.
This is where the lens of the eyes start losing its transparency (it becomes opaque or clouded ).
She said that it would probably take many years before I had to worry about it , and that when I did, the required surgery would be “routine”.
That attempt at assurance didn’t really work. I was depressed.
- Digging into my eyeballs, removing a bad lens, and putting in an artificial lens didn’t sound routine.
- I was 56, which seemed too early to get them.
- My dad and other family members have had eye issues. It seemed I was the next in line.
Amor Fati
Eventually one has to accept their fate , so I tried to lessen the worry and concern by doing the things I could do to manage my condition.
So, I tried to mitigate my cataract risks and avoid making them worse by following the National Eye Institute’s guidelines:
- Don’t
- have Diabetes.
- smoke.
- drink too much alcohol.
- have a family history of cataracts. (Unfortunately “yes” for me.)
- have an eye injury, eye surgery, or radiation treatment on your upper body.
- spend a lot of time in the sun. (I spent a lot of my childhood in the sun.)
- take steroids — medicines used to treat some health problems, like arthritis or allergies.
- Protect your eyes from the sun (shades, hats)
- Protect your eyes from injury.
- Make eye-healthy food choices. (fruits and vegetables, leafy greens, nuts, and whole grains, other)
5 Years Later
Many piles of leafy greens later but sooner than expected (August 2024), I had scheduled the first of two cataract removal operations.
I’ll tell you all about the surgery experience and decisions surrounding it , but let me first give you some interesting science and history.
What are Cataracts?
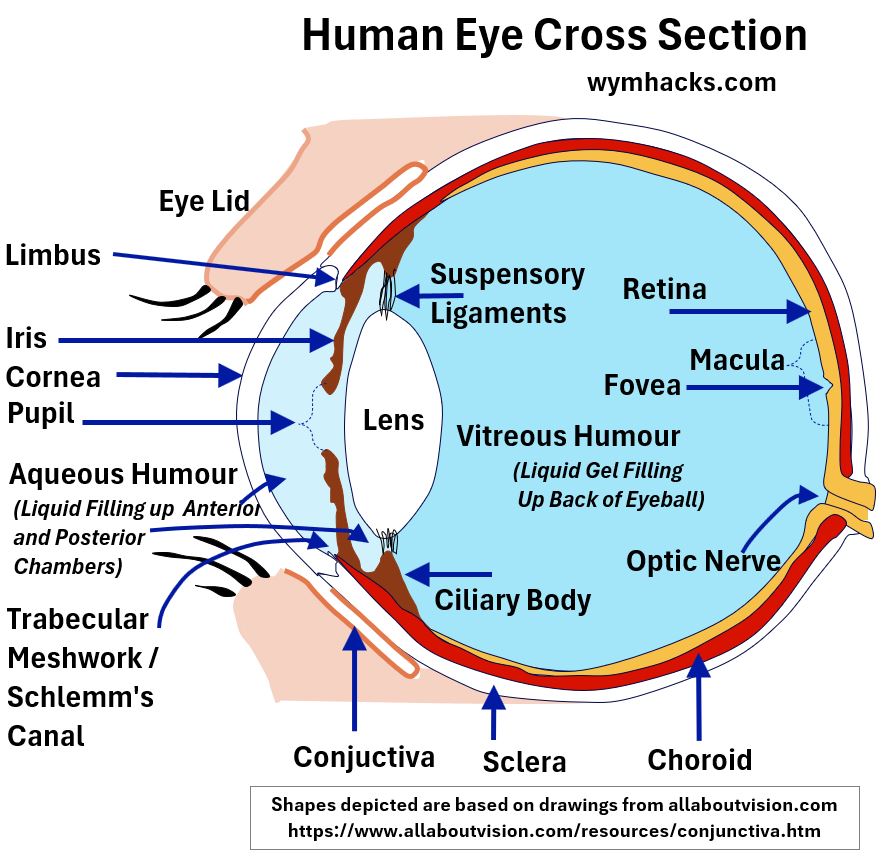
In each of your eye balls, your eye Lens is located behind the Cornea and Iris.
Cataracts occur when these Lens lose their transparency and become cloudy or otherwise discolored.
Al Ma’ Al Na’zilah (Arabic: The Descending Water)
The word cataract comes from the Latin “cataracta” which means “portcullis” (a heavy vertically closing gate made famous by medieval castles).
- It also means waterfall. (i.e. a white sheet of water cascading downwards)
- The Greek source of cataracta is katarassein which means to “dash down”.
- Some reasons for why cataracts are named as such are:
- They often look like the white of a waterfall.
- Cataracts were theorized (in ancient times) to be caused by the flow of fluids (humours) across the eye.
- They shut down access to vision like a portcullis shutting access to a castle.
The word “cataract”, used as a specific medical term to describe the affliction, was probably adopted in Europe in the 14th century (i.e. 1300s AD ).
Here’s a summary of one author’s reasonable description of how this happened (Source: 2001 , Cataracts and Hernias: Aspects of Surgical Practice in the Fourteenth Century by McVaugh):
- In the late 11th through 13th Centuries, Europeans translated Muslim scientific works from Arabic into Latin.
- The Arabic term for cataracts was Al Ma Al Nazilah (Arabic for “descending water”).
- This was most commonly translated into Latin using the word “aqua” (water),
- However, Constantine the African (late 11th century), translated it to “cataracta” and by
- the 1300s (14th century) it became the standard medical term.
Cataracts Form on the Lens of the Eye
Take a look at the image of the front of the eye below.
The white circle in the middle is the visible portion of a discolored, opaque Lens.
Picture_Eye Cataract (Front View)
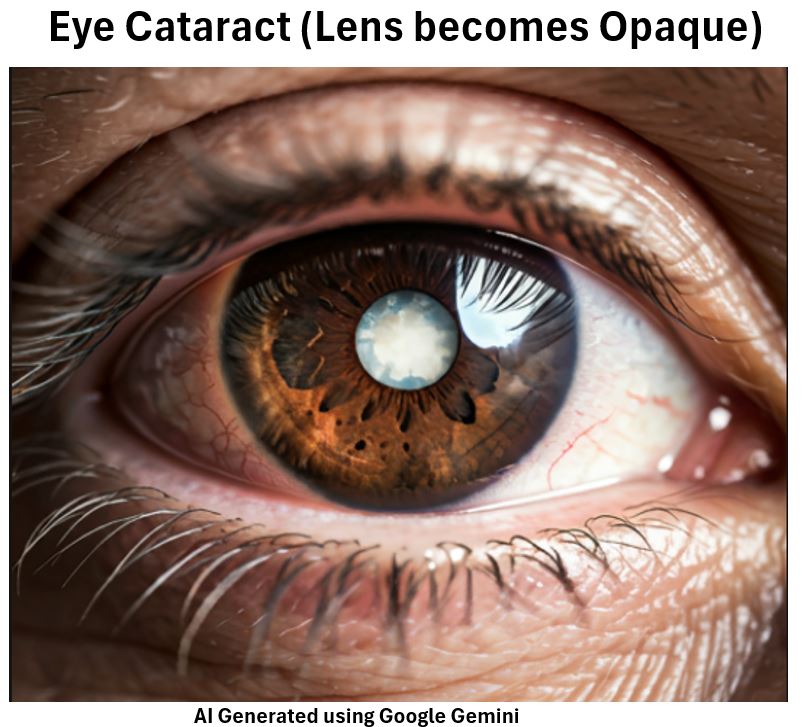
You are seeing it through the transparent Cornea and through the opening (Pupil) of a brown colored Iris.
The lens , ensconced “behind” the Cornea and the Iris, is transparent in a normally functioning eye.
Look at the schematic below for a side view of two eyeballs.
Picture_Side View of Normal Eye and Eye with Cataract
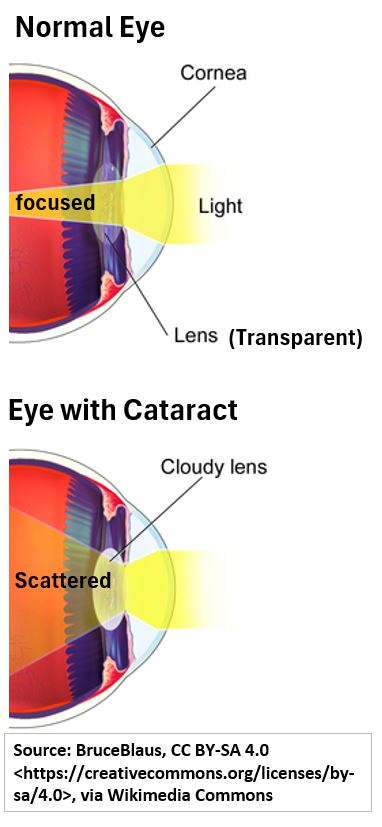
- through the transparent Cornea,
- through the opening (Pupil) of the Iris,
- through the transparent Lens, and then
- into the back of the eyeball where it is focused into an image.
For an eye with a cataract, the lens has lost some or all its transparency (it has become cloudy or otherwise discolored).
In this depiction at least , some light is getting through but is getting scattered as it enters the back of the eye.
This can cause blurry vision, haziness, and a general loss of lush color perception.
In severe cases, cataracts can cause complete loss of sight.
Types of Cataracts
Source: NEI – National Eye Institute
According to the NEI, there are 5 types of cataracts:
- Age-related cataracts (are the most common)
- They can form anywhere on the lens: inner (Nucleus), outer (Cortex), or back (Posterior Subcapsular)
- Radiation cataracts (from sun UV radiation)
- Traumatic cataracts (from injuries)
- Pediatric (younger people) cataracts formed at birth (congenital) or later on.
- Secondary cataracts (an after-cataract-surgery condition where the back capsule of the lens discolors).
I’m guessing that an age related condition could be exacerbated by additional environmental conditions like being outside in the sun all day.
Who Gets Cataracts?
Well, we hinted at it in the previous section.
Cataracts are more common the older you get.
According to the National Eye Institute, “more than half of all Americans age 80 or older either have cataracts or have had surgery to get rid of cataracts.”
According to the CDC, “Cataracts are the leading cause of blindness worldwide and the leading cause of vision loss in the United States.”
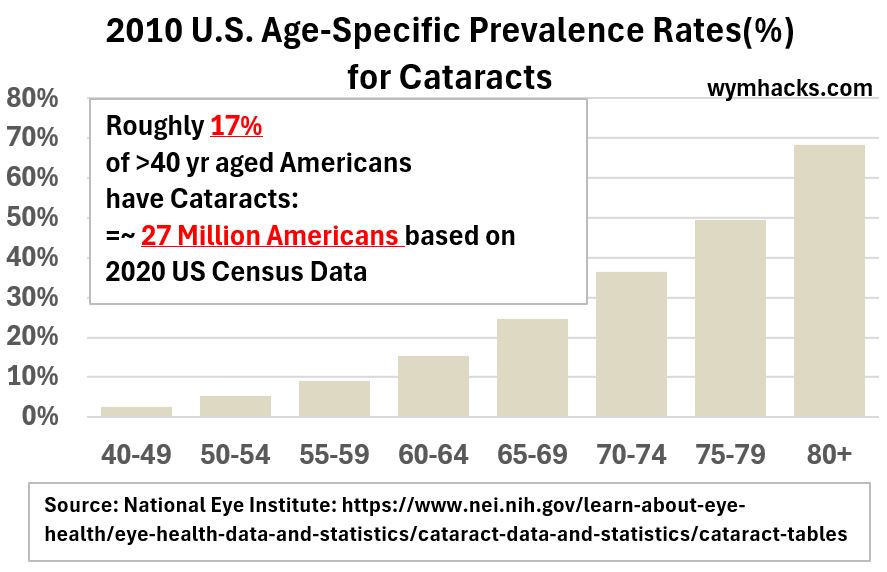
Check out the graphs below which plot the prevalence of cataracts in different age groups (based on 2010 data from the National Eye Institute; it’s a bit outdated but still valid and indicative.)
- Roughly 17% of the >40 year aged US populations have cataracts (that’s about 27 million Americans).
- Cataract rates increase exponentially with age
Picture_2010 US Age Specific Prevalence Rates (Total)
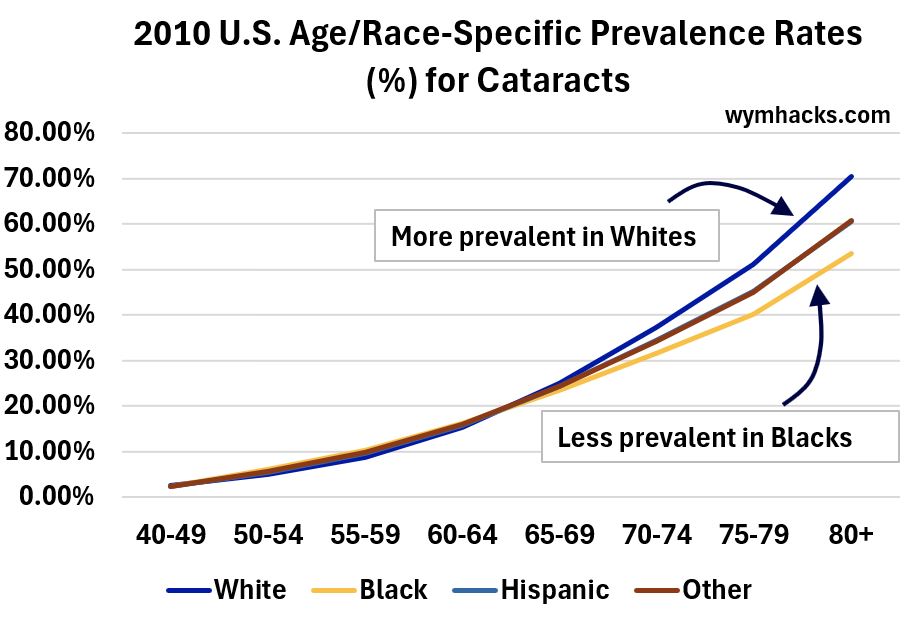
The graph below breaks down the same data by race.
- In later age cataracts seem to be more prevalent in Whites than Blacks.
- Big Question though: Is this due to socio-economic reasons or genetics or something else?
Picture_2010 US Age Specific Prevalence Rates (By Race)
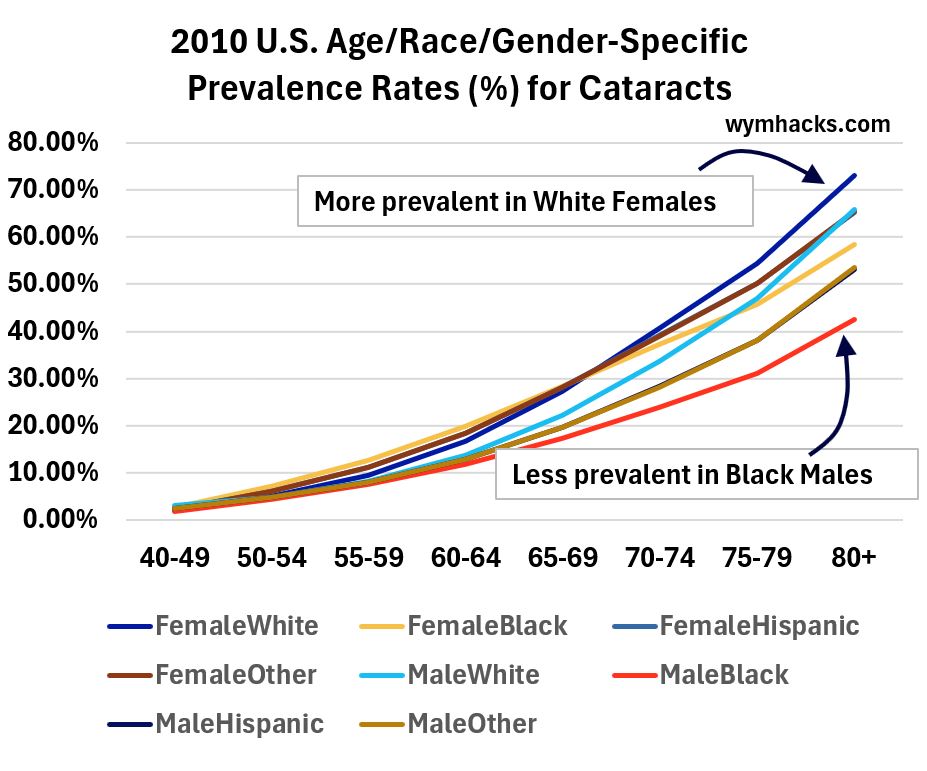
The graph below breaks the data down further by gender.
- Cataracts seem to be more prevalent in White Females.
- Cataracts seem to be less prevalent in Black Males.
I’d need to dedicate another study to really understand this data but I’m thinking that socio-economic factors might significantly influence it i.e Socio-Economic level and access to and use of medical care/intervention.
Picture_2010 US Age Specific Prevalence Rates (By Race/Gender)
Global Statistics
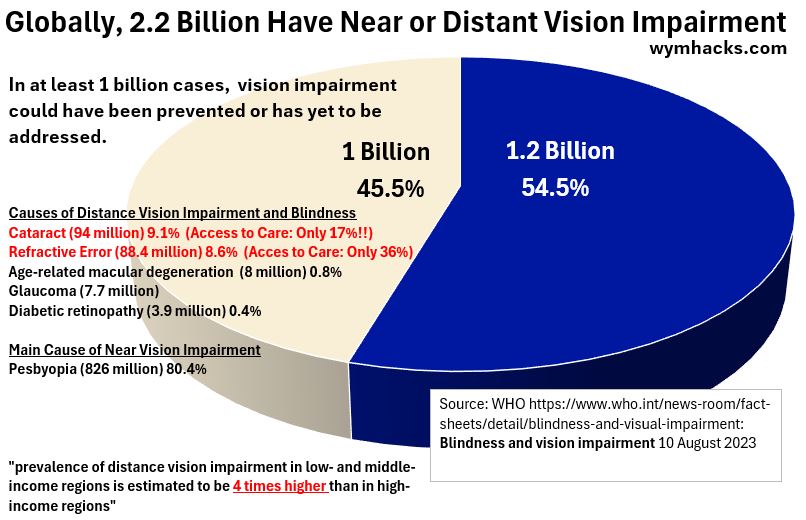
According to the World Health Organization (see graphic below),
- there are 2.2 Billion people who have near or distant vision impairment, and
- in at least 1 Billion cases, it is estimated the impairment could have been prevented or had not been addressed.
Picture_WHO Data on Global Vision Impairment (2.2 Billion People; ~ 27% of World’s Population)
Picture_WHO Data on Global Vision Impairment (About 1 Billion Could Have or Need to be Helped )
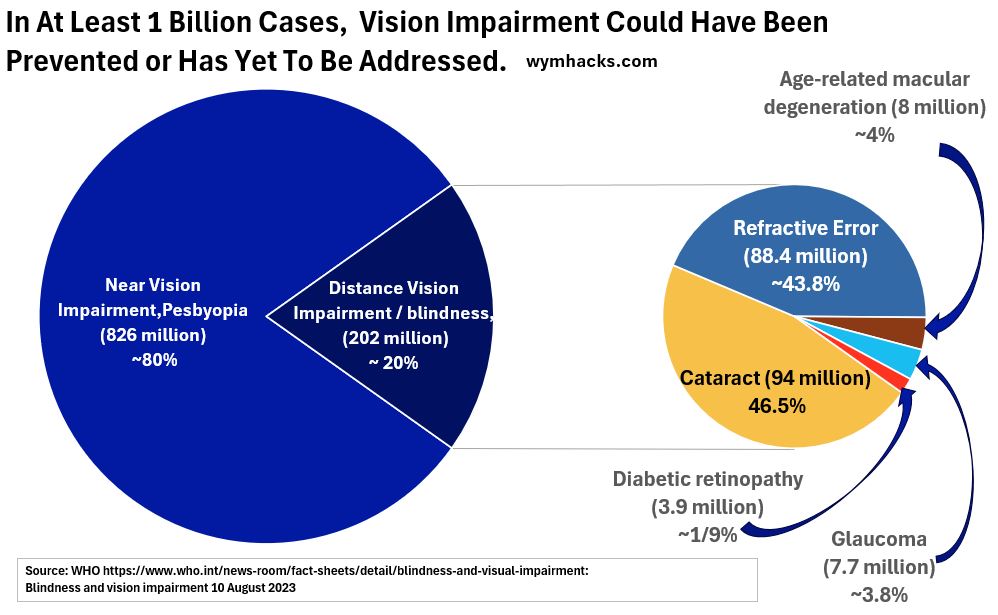
This is sad and shocking and underscores the continued need for charitable investments in eye health initiatives.
Ok, you have a feel for what cataracts are (fuzzy, hazy eyeball Lenses) and how prevalent they are (very; especially as you age).
While exploring my cataract surgery options, I found out that I could do vision corrective surgery at the same time.
Before I describe the procedure that I underwent, I thought I would provide, for the deeply curious, information on some common eye impairments and the science behind them.
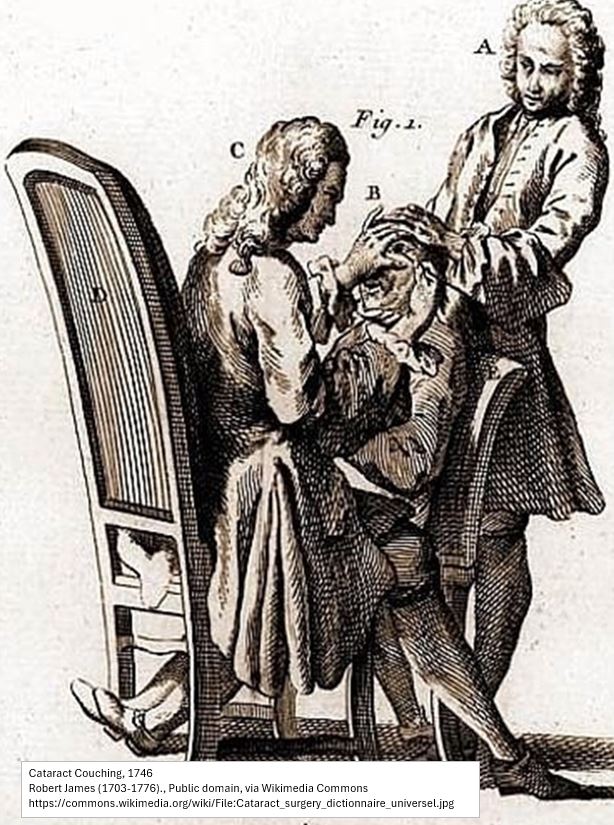
Couching
Cataracts have afflicted people throughout history.
From times before Christ all the way to the early 1800s, the most commonly practiced way to treat cataracts, called “Couching”, was pretty horrific.
Let’s imagine a Frenchman living in Paris in the early 1700s who is practically blind due to cataracts.
A cross sectional picture of one of this man’s eyes would look like the drawing below.
We’ll assume both eye lenses are so opaque , this poor Frenchman can hardly see anything.
Picture_Eye Cross Section
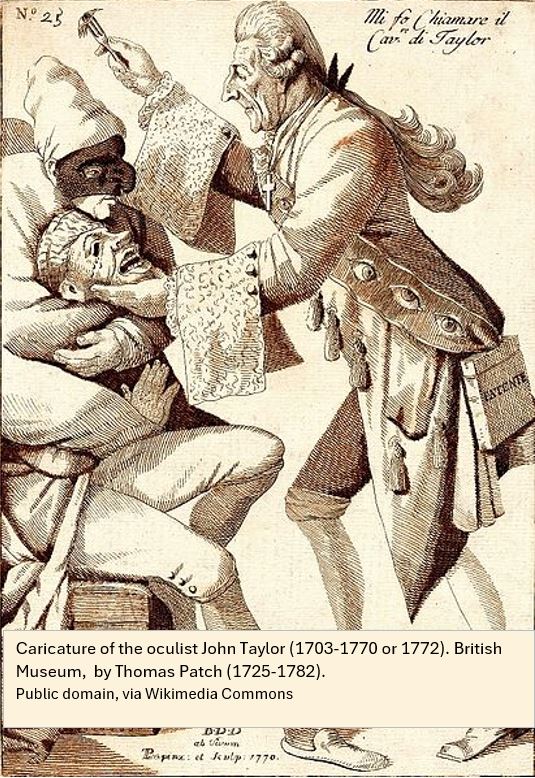
It just so happens, with great advertising glitz and fanfare, that the famous itinerant British cataract coucher “Chevalier” John Taylor is in town.
The Frenchman considers himself quite fortunate to have secured an appointment with this famous and highly respected surgeon.
On the agreed to day, the honorable John Taylor shows up at the Frenchman’s residence and performs the cataract couching procedure:
- A sufficiently strong assistant restrains the Frenchman from the back.
- John Taylor straddles the Frenchman.
- John Taylor inserts the sharp end of a metallic surgical instrument into the eyes of the Frenchman
- Taylor sufficiently agitates the instrument such that the whiteness in the eyes disappear.
- The surgical instrument used (most likely) insufficiently sterile (clean).
- The environment in which the surgery takes place is definitely insufficiently sterile.
- The poor Frenchman has not been given any anesthetic (not invented yet). He has endured great pain.
- Shortly after the procedure, with the patient still bandaged up, John Taylor makes a quick departure, claiming success.
Picture_Typical Set Up of a Cataract Couching Procedure
Picture_Cataract Couching
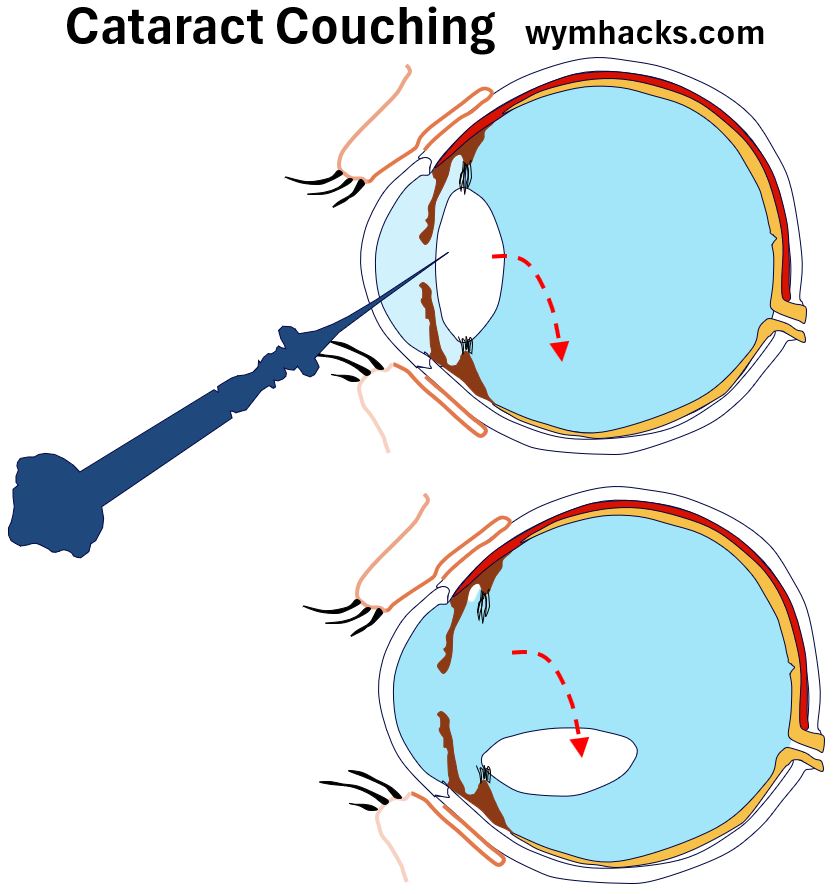
Since the Lens provides about 30% of the focusing power of the eye (the Cornea provides most of the rest), a patient with couched cataracts would definitely not see clearly but that’s still better than being blind.
The big problem was that without modern surgery conditions (for sterility) and with the crude techniques used, inflammation, infection, and other eye damage were highly likely.
This often resulted in worse conditions or even complete blindness.
The name Couching comes from the French word “coucher” meaning “to put to bed”.
I’m not sure whether “put to bed” refers to the patient or the lens.
But, we can definitely agree that this was a crude, and low probability-of-success procedure.
And it must have hurt like hell without Anesthesia!
Here are two really entertaining descriptions of cataract surgery in the good old days.
- (Video) Gross Science – The Horrors of Ancient Cataract Surgeries
(Podcast) Cataracts – Sawbones A Marital Tour of Misguided Medicine
The Charlatan Chevalier John Taylor (1703 – 1770 or 1772)
Speaking of entertaining.
The account described above is fictional but the Chevalier John Taylor is not.
John Taylor was a British eye surgeon and one of the many itinerant cataract couchers who travelled and practiced all over Europe.
He was a self-promoter and medical quack who maimed hundreds of people across Europe.
Through British royalty connections, he was able to couch many patients, some of which were quite prominent.
He is best known for couching and eventually blinding (eventually killing?) two famous musical composers: George Frederic Handel and Johann Sebastian Bach.
The excerpted sentences below are from this great article: https://todayinhistory.blog/2021/11/03/november-3-1752-quacks/
- He called himself a knight (Chevalier) and was “Flamboyant, egotistical and utterly without principle”.
- Taylor would “ride into town in a horse drawn carriage painted with images of eyes and the words qui dat videre dat vivere (giving sight is giving life), painted on the side.”
- “…patients of this Baroque era …pitchman were instructed to leave the bandage on for seven days, plenty long enough for the good doctor to get paid, and leave town.”
- “When he wasn’t busy writing his two-volume autobiography “The Life and Extraordinary History of the Chevalier John Taylor”, Taylor would ride into town and deliver a speech on a street corner before performing surgery.”
- “On the street corner. In an age before anesthesia with little conception of bacteria the idea was to get in and out, as quickly as possible.”
Picture_Caricature of John Taylor
You can read/view these entertaining pieces on the Chevalier!
History Of Cataract Removal Procedures
Couching was the predominant technique (to treat cataracts) all the way to the 1700s but, sadly, it’s still performed in some developing nations.
There were other techniques described in historical texts as well, like
- needling (discission) where the lens is essentially diced up in place
- aspiration where the lens is sucked out through a tubular syringe (ugh), and even
- extraction of the lens by incision
There were no good options in the old days and they all mostly resulted (with great pain) in bad outcomes.
Fortunately for the modern patient, significant improvements in cataract removal techniques started happening in the mid 1700s.
Eye Lens
The Lens helps focus light onto your Retina so you can see.
It’s shaped like a lentil and comprises three distinct structural parts. (Outer Capsule and inner Cortex and Nucleus).
An easy analogy describing its structure, is an M&M.
The hard chocolate outside would be the Capsule and the soft chocolate on the inside is everything else.
Picture_Eye Lens
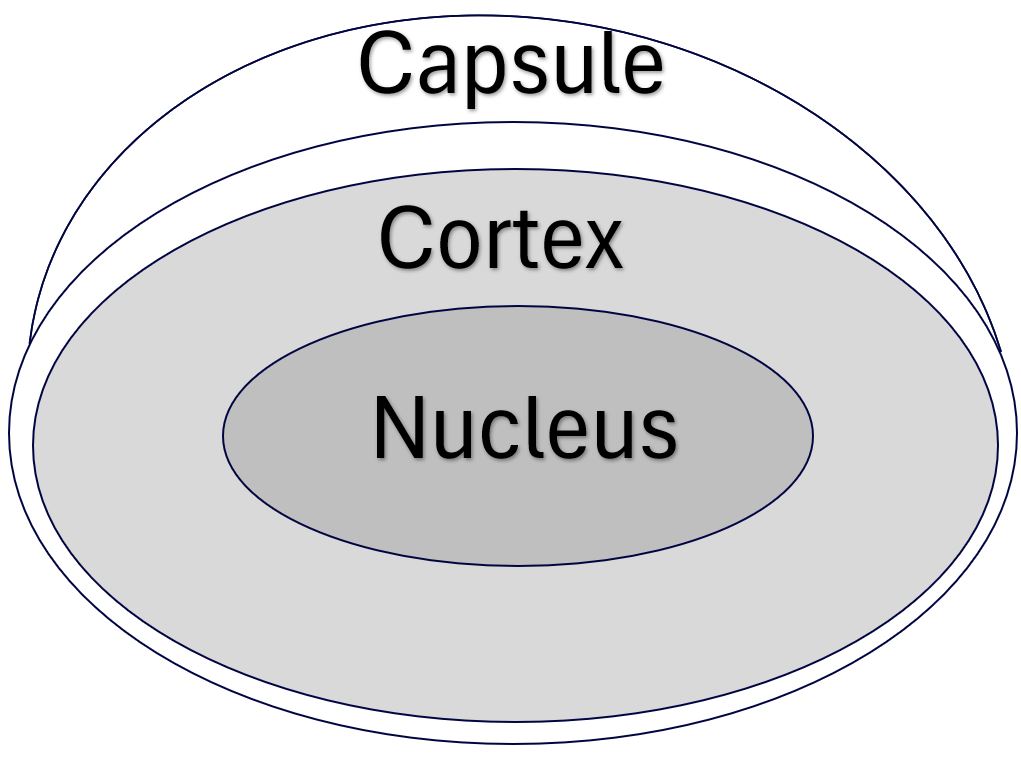
You can read more about this in my post Eye Lens Anatomy.
There are generally two types of cataract extractions that are done today, an ECCE or an ICCE.
- ECCE – Extracapsular Cataract Extraction – The Lens shell or Capsule is left in place; the insides are removed.
- This is how cataracts are typically removed today.
- ICCE – Intracapsular Cataract Extraction – Removes the entire lens of the eye, including the Capsule.
- There might be special cases where this type of procedure is done, but otherwise, ICCE is rarely performed.
IOL – Intraocular Lens
IOLs are artificial lenses (made of acrylic or silicone) that are implanted in the eye to replace the eye’s natural lens.
They are soft and foldable so they can be inserted through very small incisions.
In a typical modern ECCE, the IOL is inserted inside the lens Capsule (where in a previous step the “insides” of the lens have been “hollowed out”).
Those “arms” you see in the picture below, allow it to firmly anchor in the Lens Capsule.
IOLs are often designed for either single vision focus (near or far), or multi focus (near and far to an extent).
You can learn more about IOL types here.
Picture_Intraocular Lens IOL

Chronological Listing of Key Developments in Cataract Surgery
You can check out my post Cataract Tabulated History for a more exhaustive listing of cataracts through the ages.
Listed below are some key events in the development of cataract surgery.
- 1747: Jacques Daviel: French Surgeon – Pioneered first true Extracapsular Cataract Extraction (ECCE) where lens capsules are left in place.
- 1753: Samuel Sharp; England; First to perform Intracapsular Cataract Extraction (ICCE), whereby the lens and surrounding capsule were removed in one piece.
- 1884: Karl Koller; Herman Knap; First Topical Anesthesia (cocaine) – Koller; First retrobulbar anesthesia with cocaine – Knap
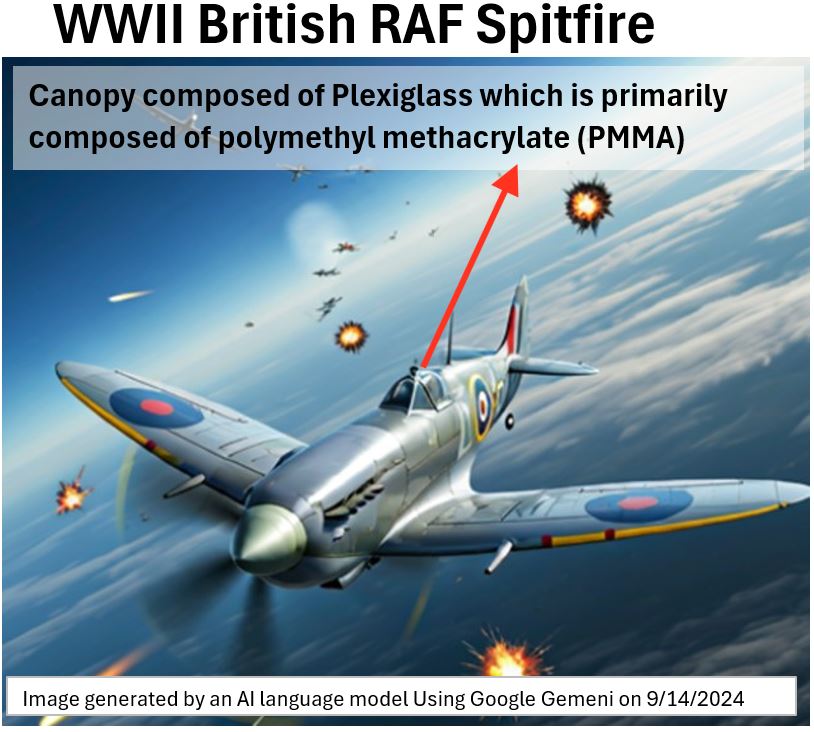
- 1949: Harold Ridley; Britain; On November 29, 1949, Harold Ridley implanted the first intraocular lens (IOL – Rayner and Keeler ltd).
- Transparent acrylic similar to RAF spitfire canopy material. Extracapsular extraction (only lens)

- 1950s-1970s: Most cataract surgeries in the 1950s to 1970s were for ICCE (capsule + lens removed).
- 1967 Charles Kelman ;USA – Small Incision Phacoemulsification procedure. Uses ultrasound. Inspired by dental ultrasound procedures.
- 1978 Kai-yi Zhou; China – Zhou implanted the first foldable IOL made of Silicone.
- 1985 Thomas R. Mazzocco ; USA – Developed refined foldable silicone intraocular “taco” lens (IOL) in 1985.
- 1993 RA Fichman ; USA – Use of topical (i.e. drops) anesthetics.
- 1995-1997 Ron Kurtz, Tibor Juhasz ; Developed the IntraLase Femtosecond Laser at the University of Michigan in Ann Arbor
- 2011 Femtosecond Laser Assisted Cataract Surgery FLACS (LenSx, Victus, LensAR, Catalys)
I highly recommend you watch these two really interesting videos describing cataract procedures through the years:
Modern Cataract Surgery Has Come A Long Way
Ok, relax, those terrible cataract couching days are gone (not entirely though ! ).
So (in general), no more getting your lens jabbed out of place with a needle without anesthetic.
According to crstoday.com (Jan 2025), “Cataract surgery is one of the most common and most successful surgical procedures worldwide, with more than 30 million performed annually.”
It’s a very accurate and safe procedure these days with a very high success rate (95 – 99% perhaps):
- The cataract surgery involves minimally invasive incisions, often done by very accurate lasers.
- Lasers can also break up the natural lens to facilitate its removal
- The traditional phacoemulsification technique (using ultrasound) is also excellent and reliable.
- The artificial lens (IOLs) are foldable and expandable such that they can be inserted through very small openings.
- The incisions typically self heal (no stitches).
- The IOLs are sophisticated and can be designed for single or multiple focus distances.
- Topical Anesthetics (along with some nice relaxants) are used and the procedure is very quick (and usually painless).
- Cataract surgery is an outpatient procedure (no hospital stay).
- Recovery is quick and clear eye site resumes in hours to a day or two.
- Days, Months, or even years after cataract surgery, a high % of people develop Posterior Capsular Opacification or PCO which can result in blurred vision.
- This is easily corrected in the Ophthalmologist’s office using a device called a YAG Laser.
- See my post Eye Lens Anatomy.
Before I describe a typical cataract surgery, let’s discuss some of the preparatory work you should do to ensure
- you have a good outcome and
- you have a reasonably good experience achieving that outcome.
Pre-Cataract Surgery “Homework”
There is a lot of good material on the web to learn all about cataract related issues including surgical options.
I think Dr. Joseph Allen does a good job deconstructing eye related issues in his videos.
- For a nice introduction watch his video: The BEST Cataract Surgery Lenses Options
- If you search for “cataract” on his You Tube site, you’ll find some other nice videos as well.
When I first started sensing and noticing the presence of cataracts, I started looking around and trying to find answers to a lot of questions like:
- which doctor to use.
- what my surgical options were.
- what insurance would pay for.
- the post insurance , out of pocket cost.
- etc.
Give yourself adequate time so you don’t rush the decisions you’ll need to make (i.e. start doing your homework before your cataracts get real shitty).
How Do You Find The “Right” Ophthalmologist?
Cataract surgery doctors (Ophthalmologists) are a highly skilled lot (years of standard medical school followed by specialization).
You’ll probably spend more time looking for the right personality fit than whether they are competent or not.
Read this National Eye Institute (https://www.nei.nih.gov/) on Finding an Eye Doctor
- Ask your trusted friends.
- I got about 5 or 6 names this way.
- Get as much information about their experiences as you can
- Ask your optometrist , especially if you’ve been using him/her awhile and you have a trusting relationship
- Ask for advice on how to go about finding the right ophthalmologist
- I found my Ophthalmologist through my optometrist
- Get Information from reputable sources on the web (US an AI tool to help you; e.g. Google Gemini or Chat GPT)
- Use the American Academy of Ophthalmology’s (https://www.aao.org/) Find An Ophthalmologist tool.
- There are several “best of” lists out there but I didn’t find them that useful.
- It was hard for me to tell if these were objective lists or just advertisements
- Ask your Health insurance provider
Ok, so you have a list of potential ophthalmologists to use.
You need to do a little vetting now.
You can find some of the answers to the questions below on-line but you definitely need to
- go meet these guys/gals face to face and
- be prepared to ask all the questions you need answers to.
Verify The Ophthalmologist’s Credentials
Ophthalmologists have to go to Medical School and then specialize. You should expect them to be highly skilled and competent individuals.
You’ll probably be able to get all their credentials from their web sites.
- Board Certification: Check if the ophthalmologist is board certified by the American Board of Ophthalmology (ABO).
- Board certification by the ABO means they’ve met rigorous standards and passed comprehensive exams.
- You can verify this at the ABO website https://abop.org/ . Choose the Verify a Physician tab.
- Where did they go to Medical School and where did they do their Residency? Can you verify that their training has a strong foundation in ophthalmology?
- I can’t speak to Foreign Medical Schools, but I believe that US Medical schools in general are known for their rigor and excellence.
- Do they have Fellowships and Subspecialties in the area of cataract surgery?
- Verify they have a State Medical License (check your state’s medical board website.)
Verify The Ophthalmologist’s Experience and Patient Feedback
- How many cataract procedures has your doctor performed? Ask them this during your face to face.
- Fewer doesn’t mean bad but the more procedures done, the better.
- Ask him what his success rate is for cataract procedures?
- One told me 95% and one told me 99%. Which one would you choose?
- Patient Reviews: Does your ophthalmologist track his own patient’s feedback? He / She should I think.
- Check the doctor’s patient reviews on his/her own web site. Are there any bad ones?
- Use online doctor rating sites: Read this web md article : How to Use Online Ratings for a Doctor
- These can be misleading and not necessarily objective , but
- it’s additional data you can collect and then verify / discuss with the doctor if you have any concerns
What is the Ophthalmologist Like Face to Face?
- Honestly, for me , this was one of the most important questions to answer.
- I needed to make sure the Ophthalmologist was the type of person I would be comfortable dealing with.
- Did you sense the doctor was genuine , honest, and thoughtful?
- Did he/she make time for you?
- Did he/she answer all your questions thoughtfully?
- What were the office dynamics like?
- Did the office feel like a Mill, trying to maximize volume and turnover?
- Did you feel rushed. Again, did you get the attention you needed?
- Be reasonable, there has to be a balance between their attention to you and conducting their business.
What Techniques, Technologies, and Facilities Are Used?
- The doctor will need to know your eye’s refractive issues, corneal issues, retinal issues etc..
- Make sure she has all the modern tools to do this (ask her or her staff to show you the gear)
- Is the doctor capable of working with lasers? Does he offer this option?
- What kind of IOLs (Intraocular lens that will replace the natural lens) can she install?
- If you have Astigmatism, ask if the doctor can correct this (and how) during the cataract surgery.
- For general cataract surgery, you are going to go home after the procedure (outpatient).
- Is the facility close to where you live?
- What type of center is it? Is it
- an Outpatient Surgical Center?
- a Hospital Outpatient Department?
- an Office-based surgery suites?
- a school associated surgical centers (e.g. University of Houston College of Optometry Surgical Center)?
- Regardless of the center type, does have hospital level sterility and state of the art equipment?
- Is the facility dedicated to Cataract surgeries?
- If not, that’s not necessarily bad, but I would learn more about the other ways its being used
What kind of IOLs Do You Want?
Well, this is a big decision for you.
You want to be happy with what you put into your eyeball because it’s not trivial to remove it (ask your doctor about this).
You have to really figure out what you want and what is best for you. Your doctor should help you with this.
- See this wonderful video by Dr. Joseph Allen: The BEST Cataract Surgery Lenses Options
- This aao.org article on your IOL choices is pretty good.
The Ophthalmologist should have plenty of information on your options and what he offers.
Here are some of the choices you’ll have (Your Ophthalmologist will have to determine what you are a candidate for as well) :
A Monofocal (and possibly Toric lens). A Toric lens corrects for Astigmatism.
- These will give you focus at one distance.
- A Distance focusing lens means you can see far but you’ll need glasses for shorter distances and when reading books for example (or your cell phone)
- A Near distance focusing lens allows you to see things up close (reading for example), but you’ll need glasses for greater distances
- So you kind of get an either one or the other choice here (although you can mix these for each eye; ask your doctor about this one)
A Multifocal (or Trifocal) IOL.
- These give you a much wider range of clear vision (all in one lens) – I can confirm this was true for me.
- You should be able to read a book and you should be able to see far distances clearly.
- You will see Halos around bright lights at night. These should diminish with time. (I can confirm this is true).
- You wont see things as clearly in dimly lit lighting (I can confirm this is true especially when trying to read a book – you need light).
You might have specific eye issues which require additional unique solutions, but in general,
- your main decision is: do you want a Multifocal Lens or a Monofocal Lens to replace your eye’s natural lens.
Understand What Procedures and Material Will be Covered by Your Medical Insurance
Get the exact descriptive details and associated surgical codes (if any) of all the procedures and materials you are interested in.
For example, for me, for each eye, my procedure was going to entail the following:
- Femtosecond Laser Assisted Cataract Surgery (FLACS)
- Corneal incisions for Astigmatism correction. Other descriptors for this procedure are:
- Limbal Relaxing Incisions (LRIs) – more peripheral cuts,
- Astigmatic Keratotomy (AK) – less peripheral cuts
- Arcuate Keratotomy (also AK).
- Installation of a Clareon Panoptix multi-focal lens (insert further specs as needed)
Talk to your insurer first and see what they will cover.
Make sure they understand the details of your procedure, otherwise they will give you generic information that will probably be wrong.
My experience was that my insurance covered very little of the total cost.
- Just call the insurer first, armed with the details, and get your answers.
- You’ll be discussing the pricing with the opthalmologist as well.
- With the two sets of data from your insurer and your doctor, you can compute your out of pocket expense.
A Modern Cataract Procedure
The vast majority of cataract procedures will have the basic steps described below (*).
(*) The descriptions below are based on my own experience so the sequence or some of the exact details might be a little different for your procedure.
Note that
- typically one eye is done at a time. So the steps described below will happen for each eye (if both eyes need the surgery that is).
- I did mine two weeks apart. You want some time to let the eye heal up a little and make sure everything is ok before doing the other eye.
Establishing your Tailored Cataract Surgery Plan
Your Ophthalmologist will need to know the specific conditions and measurements of your eyes.
He / She will
- determine the extent and severity and type of cataracts you have.
- measure your refractive errors (Near Sighted or Far Sighted).
- measure the shape of your eye and Cornea to determine if you have Astigmatism.
- examine your retina for any abnormalities.
- measure your eye blood pressure.
- do whatever else they need to do , given your specific eye condition.
Based on your specific eye conditions, you and the doctor will agree to an overall surgical plan which could incorporate more than just replacing the cataracts with IOLs.
These are highly personal decisions where you’ll have to balance your desires against cost.
Discuss the all the risks and possible complications also. No surprises; that’s your desired outcome.
I didn’t want to wear glasses anymore to see near or far (I am nearsighted and Astigmatic and have Presbyopia), so the doctor and I agreed on the following plan:
- use laser FLACS surgery in concert with “traditional” surgical tools to
- remove the natural lens and install a multifocal IOL designed to be able to give me both near or far vision ; and
- “correct” the cornea for Astigmatism via an Arcuate Keratotomy. For more information,
- view this nice animation by atlantiseyecare.com: limbal relaxing incision.
- see the corrective procedures section of my post : Vision Correction.
My insurance coverage did not cover much of my plan.
- I believe that insurance will typically cover phacoemulsification procedures where mono focal IOLs are used. (you just have to check)
- According to one web site , “Advanced types of cataract surgery…can average about $4,000 to $6,000 out-of-pocket, per eye.”
- I can confirm that my out of pocket cost was in this range.
Consent
Like I mentioned above, have a thorough discussion with your doctor regarding all the possible risks and corrective action for those risks.
Apparently, as high as 60% of the time, after cataract surgery, the back part of the lens capsule will shrink and cause some vision fuzziness.
- This condition, Posterior Capsule Opacification, is easily correctible at the doctors office using a laser called a YAG laser.
- See my Eye Lens Anatomy post also.
You are going to have to sign consent forms agreeing to the procedure and to the risks of the procedure.
At the surgical facility ,on the day of the procedure,
- you should confirm with the staff , your anesthesiologist, and your doctor the exact procedure you are undergoing. (i.e. which eye, what exactly are we doing, etc.).
- you’ll sign a consent form for the facility / anesthesiologist / doctor as well. This is an official agreement that you know what the procedure is and that you know and accept the risks.
Pre-Surgery Preparation – Day Before
Follow the instructions provided by your doctor to
- arrange for home transportation after the surgery (this is an outpatient surgery),
- not wear contact lenses for some period of time before the surgery.
- fast appropriately.
- ensure your face is washed and clear of makeup etc.
- etc.
Location of Surgery
You need to show up at the surgical facility at the right day and time as instructed by the doctor/facility.
Cataract procedures are typically outpatient procedures (i.e. the patient goes home after the surgery).
Facilities equipped to perform cataract surgeries can be part of
- an “eye center” associated with one or more practices,
- a private practice,
- or even a facility associated with a university like the ambulatory eye surgery center affiliated with the University of Houston School of Optometry. (This might be the only one in the US at this time).
Pre-Surgery Preparation – At the Surgical Facility
You’ll show up at your allotted time, complete the necessary paperwork and probably make any necessary payments at that time (depends on your exact procedure and what will be insured versus not insured).
Make sure you’ve read and signed all the necessary consent forms (see the Consent section above)
A friendly staff member will bring you in the preoperative area and start preparing you for the procedure.
- Typically you’ll lie down in a bed and just have your shoes off (just be in comfortable clothing).
- The nurse will
- hook you up to heart and blood pressure monitoring equipment.
- prepare your eyes with a combination of dilating, antiseptic, and anesthetic eye drops (your iris is sensitive so it needs to be numbed up).
- offer you anxiety medication like Valium.
- connect you to an I.V. (Intra Venous) drip bag (containing Versed or Fentanyl typically).
Your doctor will perform the procedure but he/she will be accompanied by an anesthesiologist and at least one nurse.
You will meet the anesthesiologist in the pre-op. area.
Be sure to ask him/her any questions about the procedure.
- The anesthesiologist will
- monitor your vitals (e.g. blood pressure, pulse, oxygen level) during surgery.
- adjust your IV to reduce and control your anxiety/pain during the operation.
The desire is to have you awake during the procedure so you can provide feedback regarding pain or other discomfort etc.
The Surgery
Ok, you are prepped up, drowsy and dreamy but awake.
You now get rolled into the operating area.
The eyeball they are gong to work on might look a little like the cross sectional drawing below.
Picture – Cross Sectional Layout of Front of Eye

In the following steps, the surgeon might do the whole procedure manually or he might use a sophisticated laser tool to do some precision cutting and incisions.
With the eye numbed and ready for surgery,
Make a Circular Opening through the Capsule of the Lens
- Anterior Capsulorhexis: A circular opening is created in the Anterior Capsule of the Lens.
- In the drawing below I show this being done manually with a surgical instrument (in my procedure, this was done with a laser).
- The instrument is inserted through an incision made near the boundary area of the Cornea (called the Limbus ; see my Lens Anatomy article).
- If a laser is used, it is also used to create an incision near the Limbus because the surgeon needs access to remove the natural lens remnants and to insert the IOL.
Picture – Anterior Capsulorhexis (remove top of lens capsule)
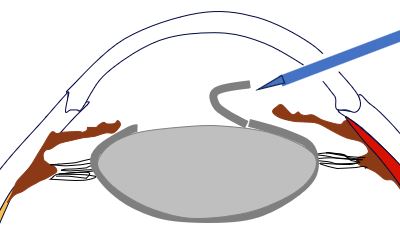
- Other corrective procedures can be performed at this time as well.
- For example, incisions can be made in the Cornea to reduce or eliminate Astigmatism (irregularly shaped Cornea).
- I describe these in more detail in my Vision Correction article.
- The same laser machine that the doctor uses for the cataract surgery can be used to make the corneal incisions.
- These Corneal incisions for Astigmatism are also called
- Limbal Relaxing Incisions (LRIs) – more peripheral cuts,
- Astigmatic Keratotomy (AK) – less peripheral cuts
- Arcuate Keratotomy (also AK).
- Clear Corneal Incisions
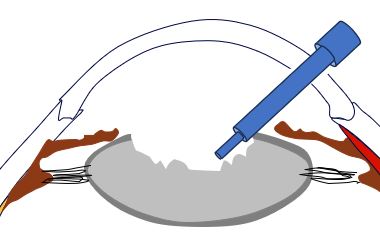
Dissolve/Breakup The Lens Internals
- Phacoemulsification: “Phaco” comes from the Greek word “phakos,” which means “lens.”.
- An ultrasonic probe is inserted through the small incision.
- This probe uses high-frequency sound waves to break the cloudy lens (cataract) into tiny pieces.
- I show a phacoemulsification instrument in the drawing below.
- If a laser is used, the laser will fragment the lens internals such that the material can be easily removed by the surgeon.
- The dissolved or softened or emulsified lens internals are sucked out by the surgeon.
- When a laser fragments the lens, the phacoemulsification tool is still used to remove the lens “guts” but power use and time required is significantly reduced.
Picture – Removal of Lens Internals
Insert the Foldable IOL into the Lens Capsule “Shell”
The surgeon, once he has cleaned out the internals of the natural lens, uses a special instrument to place a foldable IOL into the Lens Capsule Cavity.
Picture – Insert the IOL into the Lens Capsule
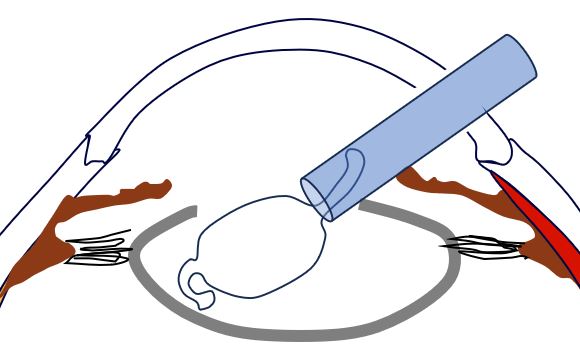
The IOL expands into the Lens Capsule space, and the arms of the IOL serve as anchors to fix the lens.
The incisions (cuts) required to insert the instruments and to insert the IOL are are so small that typically no sutures are needed.
Once the procedure is finished, the cuts close up and begin to heal naturally (no stiches required).
Now, take a look at this video which visually summarizes what I’ve described above:
- Cataract surgery with Laser Lensx™
- This video is an advertisement for the Alcon Lensx laser technology that my surgeon used.
- I’m not being paid to endorse these guys; the video just provides really nice cataract surgery animations .
- This technology is generally called Femtosecond Laser Assisted Cataract Surgery or FLACS.
- FLACS employs extremely short pulses of light which make precision cuts with minimal damage to surrounding tissue.
- Some of the commercial FLACS providers are LenSx, Victus, LensAR, and Catalys.
Post-Operation
The whole process above might take 15 or 20 minutes.
You will have been awake during the procedure but depending on the medication you take, your concept of time and what exactly transpired will be a bit “fuzzy”.
You will get rolled out into a post-operational area, and you’ll be observed for a little bit before you are ready to leave.
A spouse, relative, friend will need to be there with to get you and drive you home.
Your doctor will have given you post-operative instructions so just follow these.
- You will have your first check up with the doctor the day of or the following day from your surgery.
- You’ll have a few more checkups scheduled in the next 30 days. (I think it was one after 1 week and one after 30 days for me)
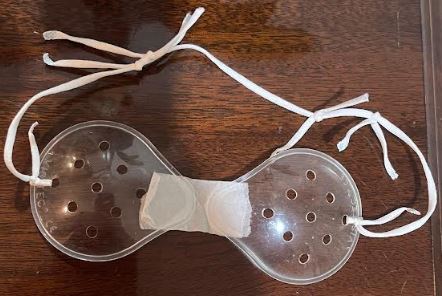
- You will wear a transparent protective eye shield.
- It’s there to prevent you from rubbing or otherwise touching your eyes (especially when you sleep).
- Generally you’ll wear these at night. (I didn’t wear mine during the day but I stayed mostly inside the house for the next 2 or 3 days).
- Your eyesight will be blurry for a few hours but should start to clear up pretty quickly (within several hours post surgery for me).
- You should (I think) be given anti bacterial drops. Apply these exactly as instructed,
- One of your biggest risks is infection. Apply the drops religiously. Don’t mess around.
- Avoid having water or other things contact your eyes for at least two weeks after the surgery. Don’t swim. Don’t put shower or wash water in your eyes.
- Avoid working out for at least a week (you want to avoid any strain on your eyes).
Conclusion

Today, Cataract surgery is safe and one of the most common surgeries done in the world.
Sadly, many people still don’t have access to it and some, horribly, still undergo some variation of the ancient couching technique.
Hopefully you will have recourse should you develop cataracts:
- Give yourself time to learn about Cataracts ,Cataract removal procedures, and (IOL) Intraocular Lens types.
- Find a well thought of Opthalmologist and work with them to design your exact surgical procedure/s.
- Consider other procedures (like Astigmatism correcting surgery) that can be done at the same time as the cataract surgery.
- Understand the cost and the risks involved.
Epilogue
It’s been about 5 months since my cataracts were removed.
I’m really happy (so far!) with the Multifocal IOLs that are now sitting in the natural lens capsules of my eyes.
- I don’t wear my progressive lens glasses anymore
- I can run, swim, drive, etc.. unencumbered by glasses and with 20/20 vision
- I changed out my sunglass lenses to non prescription lenses.
- Yes, I do see halos on lights at night, but they are slowly diminishing
- This doesn’t bother me, but if you are doing a lot of night driving it could.
- Yes, it is harder to see up close if I don’t have sufficient light.
- I am still trying to optimize my physical book reading.
- I’m still trying to adjust the optimal distance of the book from my face when I read.
- The room lighting now makes a big difference. The more light, the clearer the reading.
- Reading books on backlit electronic devices works well
Of course, you might be perfectly happy with Monofocal IOLs and using glasses to correct for either near or far vision.
But, let’s all agree that, no matter the specific options chosen, Cataract Surgery is an amazing modern medical marvel which gives “Light After Darkness“.
Disclaimer: The content of this article is intended for general informational and recreational purposes only and is not a substitute for professional “advice”. We are not responsible for your decisions and actions. Refer to our Disclaimer Page.