Menu (linked Index)
The Immune System – A Primer
Last Update: August 22, 2024
Introduction
Your Immune System employs amazing defense mechanisms that protect your body from disease and sickness.
This article describes the various cells, proteins, and organs that make up the Immune System and how they work together to keep us safe from “bad actors” including:
- Pathogens: Bacteria, Viruses, Fungi, Parasites
- Toxins: poisonous substances produced by living organisms
- Allergens: cause an Immune System “over-reaction” (e.g. dust, pollen)
- Foreign substances: poisons, chemicals, even objects like a splinter
- Internal abnormalities: (e.g. cancerous cells, transplanted organs)
We’ll review
- Innate (born-with) immune responses and Adaptive immune responses.
- the different types of White Blood Cells (WBC).
- how WBCs innately and adaptively battle bad actors.
- the systems in which WBCs operate.
- the importance of vaccinations.
- Immune System disorders.
- habits and nutrition for maintaining immune health.
I hope this article sparks your curiosity and sense of wonderment and whets your appetite for further discovery!
Acknowledgement: I watched and re-watched the Khanacademy videos listed below. If you want to get a nice, “clean” understanding of the topic, I would advise you do the same.
Khanacademy.org Videos on Immune System
- Innate immunity(document)
- Adaptive immunity(document)
- Role of Phagocytes in innate or nonspecific immunity
- Types of immune responses: Innate and Adaptive, Humoral vs. Cell-Mediated
- B Lymphocytes (B-Cells)
- Professional Antigen Presenting Cells (APC) and MHC II complexes
- Helper T-Cells
- Cytotoxic T-Cells
- Review of B-Cells, CD4+ T-Cells and CD8+ T-Cells
- Clonal selection
- Self vs. Non-Self immunity
- How White Blood Cells move around
- Blood cell lineages
Purpose of the Immune System
Protect Against Harm
The purpose of the human Immune System is to protect the body from both internal and external threats including:
- Pathogens
- Cancerous cells
- Toxins: Harmful substances produced by bacteria, plants, or chemicals
- Transplanted organs and tissues
Allergic reactions are also a type of immune response but might not always be beneficial .
In this case, in its zeal to protect you, your Immune System will misfire and over-react to Allergens (certain foods, pollen, pet dander, dust mites, etc.).
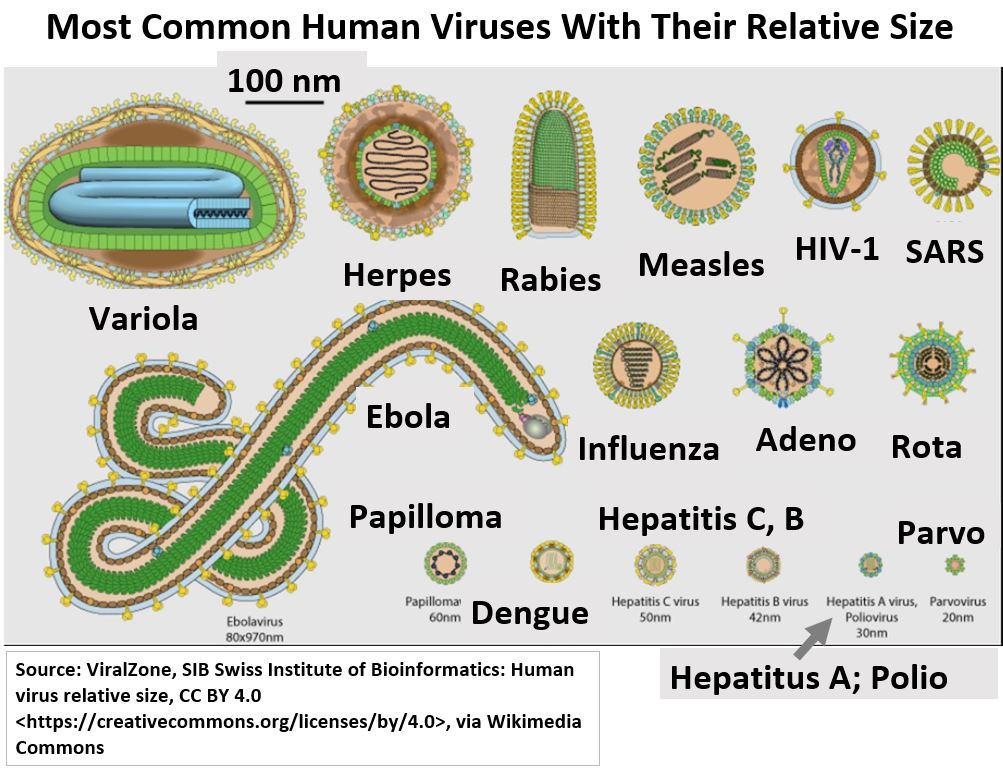
See the picture below for a picture and relative size representation of some common viruses.
Vaccinations , a testament to human ingenuity, allow our bodies to develop immunity against them.
Picture_Virus Types and Relative Sizes
How the Immune System Works
A normally functioning Immune System identifies what belongs in the body (self) versus what does not (non-self or foreign) and then acts to eliminate the threat.
The Immune System defends us by
- providing physical and chemical barriers that keep harmful substances out.
- detecting any threats.
using White Blood Cells
- in brute-force, non-specific responses (i.e. innate) to any substance sensed as “harmful”.
- in more sophisticated adaptive responses which give us immunity.
Key Definitions
Before we describe some of the key body systems that aid in the immune process, let’s get a few more definitions out of the way.
Human Immune Response Systems
Innate Immune Response
- Provides a rapid and non-specific immune response to pathogens and other bad actors.
- Includes a first line of defense against infection etc. provided by skin, mucous, acids and other “near the surface” barriers.
- Includes a second line of defense provided by certain types of White Blood Cells (e.g. Phagocytes , Natural Killer Cells, etc…).
- Phagocytosis is the process where a White Blood Cell Phagocyte engulfs, digests, and produces waste from a pathogen or bad actor (they also play a role in Adaptive Immune responses) .
Adaptive Immune Response
- Provides a slower but very specific immune response.
- Certain types of Innate Immune Response White Blood Cells (e.g. Dendritic Cells and Macrophages) also have Adaptive Immune System roles.
- Other Key players are B-Cells and T-Cells which are called Lymphocytes.
- Antigens are involved
- An Antigen is any substance that can trigger an immune response.
- This includes specific genetic markers that might exist on the surface of a virus , for example, or,
- it could be the presence of a skin cut (where the body recognizes the damaged tissue as foreign or abnormal).
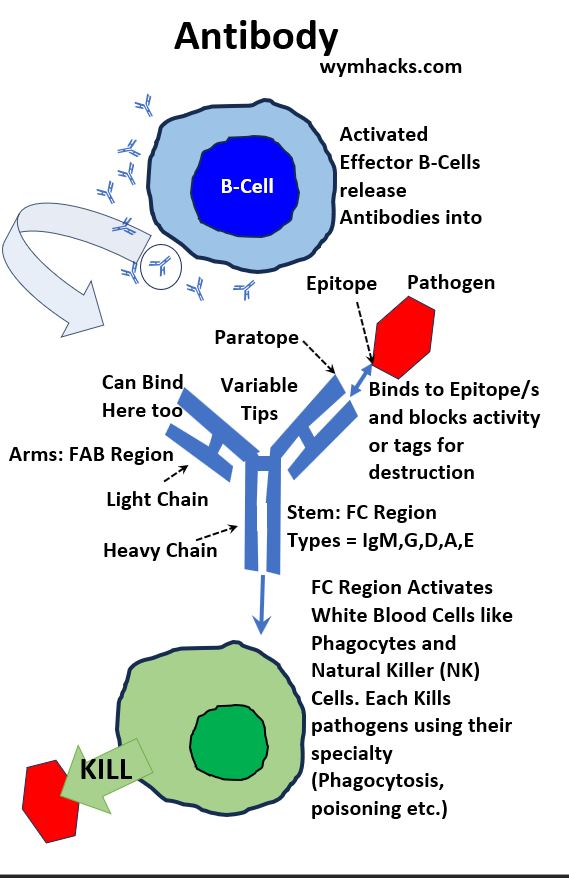
- Antibodies are involved
- An Antibody is a protein produced by White Blood Cells to help neutralize/destroy bad actors (pathogens, cancer cells, etc.).
- They are also called Immunoglobins.
White Blood Cell
White Blood Cells (WBCs) fight pathogens and other bad actors (e.g. cancerous cells).
They develop from Stem Cells which are produced in bone marrow. (See Appendix I for a chart showing Stem Cell derivatives).
- Some WBCs attack pathogens in non-specific ways (AKA Innate Immune Response) while
- others target and destroy specific bad actors (AKA Adaptive Immune Response).
- Some WBCs play a role in both immune and adaptive responses.
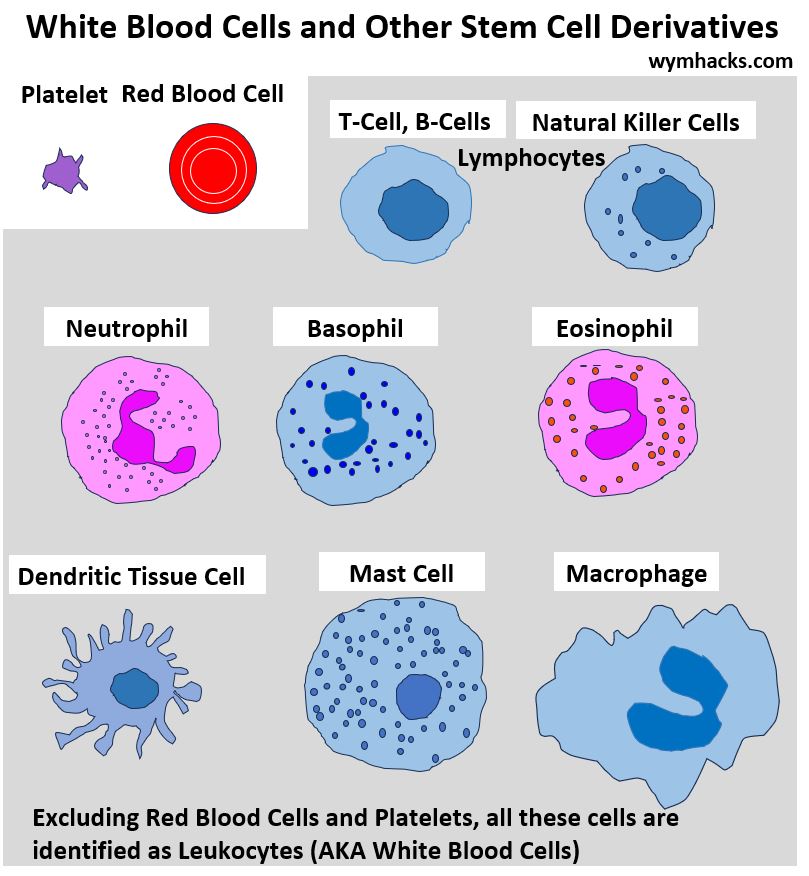
White Blood Cell Types
Picture_White Blood Cells and other Stem Cell Derivatives

- Mast Cells (Innate) release Histamine and other chemicals involved in inflammation and allergic reactions.
- Dendritic Cells (Innate and Adaptive) are Phagocytes that can also capture, process, and present Antigens to T-Cells.
- Macrophages (Innate and Adaptive): Phagocytes that can also capture, process, and present Antigens to T-Cells. Also interact with Antibodies. They last longer than Neutrophils.
- Neutrophils (Innate and Adaptive) are the most plentiful first responders that are Phagocytes and also interact with Antibodies. They die after use and produce pus.
- Eosinophils (Innate) combat parasitic infections and play a role in allergic reactions.
- Basophils (Innate) release Histamine and other chemicals involved in allergic reactions and inflammation.
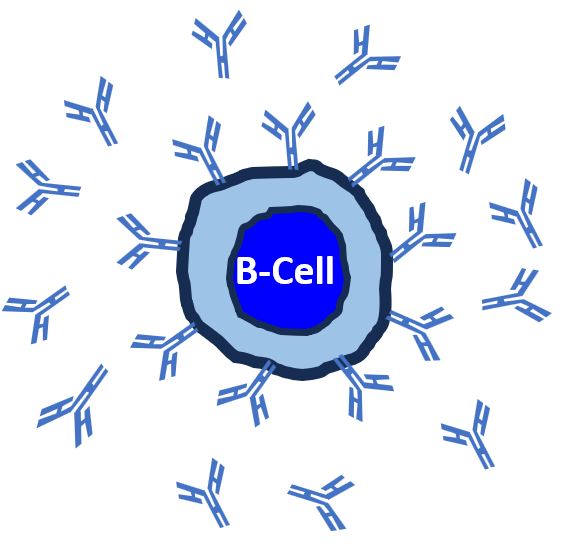
- B-Cells (Adaptive) produce Antibodies. Can present Antigens on their surfaces. Key players in the Adaptive Immune Response System.
- T-Cells (Adaptive) activate B-Cells into action and also kill infected cells, cancer cells, and foreign substances.
- Natural Killer Cells (Innate) respond rapidly to destroy virus-infected cells and cancer cells.
Where the Immune System Operates
The Immune System is a complex network of cells, tissues, and organs working together to protect against pathogens and other bad actors (e.g. viruses, bacteria, cancer, allergens etc.)
Body Systems Involved in Immune Response
The Immune System operates everywhere in the body but relies on many body systems to work efficiently.
The Circulatory System
- transports White Blood Cells to needed locations.
- provides nutrients needed by Immune System actors.
- removes waste created by immune responses.
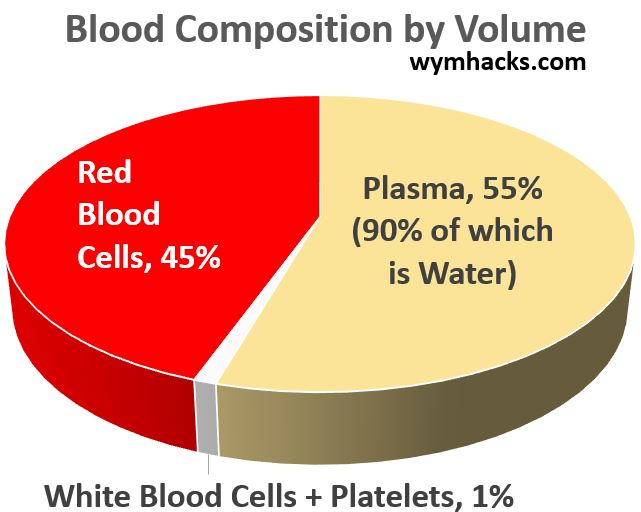
- has a typical blood composition as shown in the chart below.
Pie Chart_Blood Composition by Volume
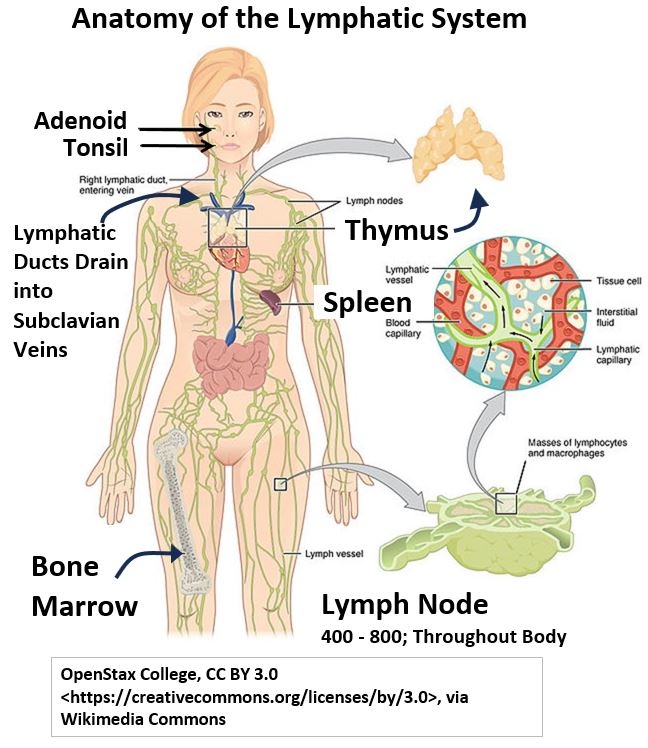
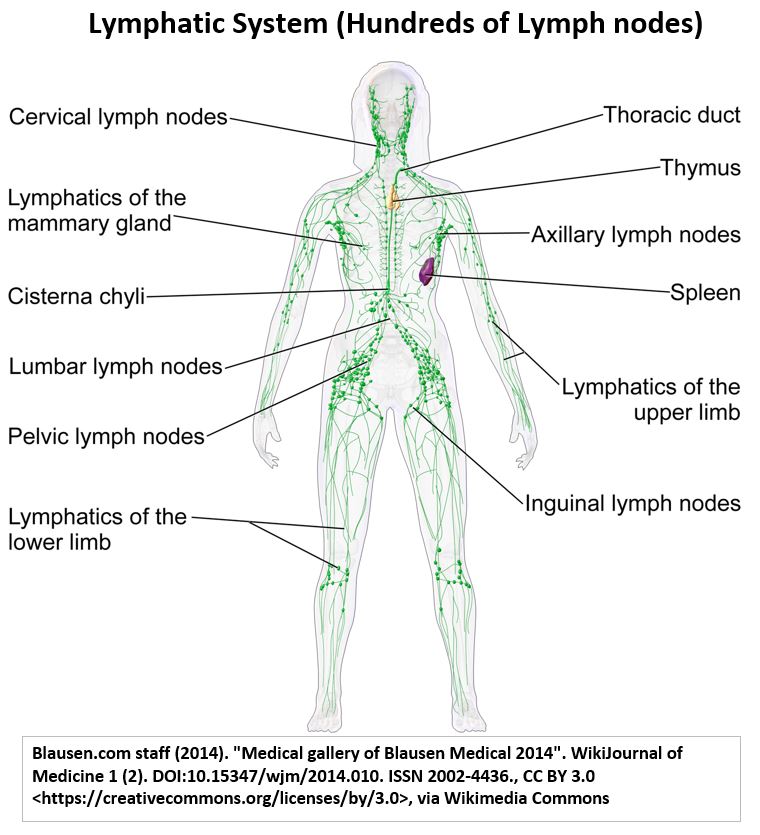
The Lymphatic System
- is a major storehouse of B-Cells and T-Cells (in Thymus, Lymph Nodes, Spleen)
- develops and matures T-Cells (in Thymus).
- is the main place where T-Cells and B-Cells are activated to perform Adaptive (specific) Immune Responses (in Lymph Nodes).
- , through its key function of body fluid recovery, transports immune cells into blood for action across the body.
- has other key roles like fluid filtration and fat absorption.
- Why we need a Lymphatic System – khanacademy.org
- The Lymphatic System’s role in immunity- khanacademy.org
- Anatomy of the Lymphatic and Immune Systems – openstax.org
Picture_Anatomy of the Lymphatic System
Here are some quick summaries of other body systems that impact the Immune System:
Respiratory System
- First line of defense: Mucus and cilia trap pathogens.
- Oxygen supply: Provides oxygen for immune cell metabolism.
Digestive System
- Nutrient absorption: Provides essential nutrients for immune function.
- Gut microbiota: Contributes to immune development and function.
Integumentary System (Skin)
- Physical barrier: Prevents pathogens from entering the body.
Endocrine System
- Hormonal regulation: Influences immune responses and inflammation.
Nervous System
- Stress response: Impacts immune function.
- Communication: Coordinates immune responses with other bodily systems.
Immune System Responses
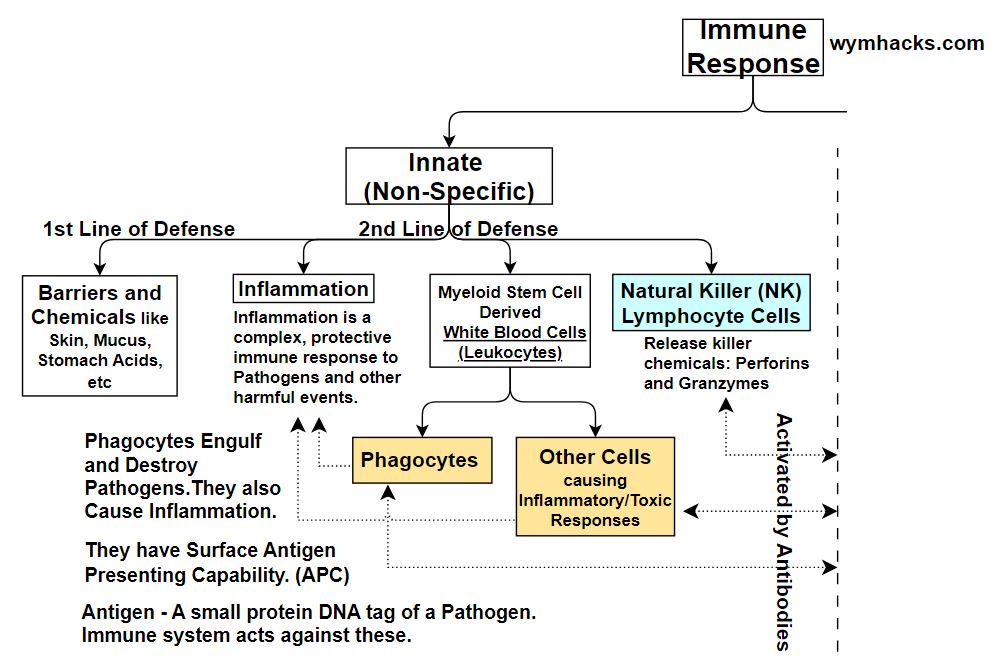
The body’s immune responses are broadly categorized as Innate or Adaptive.
- Innate Immune Responses are “born-with” non-specific and tend to happen quickly.
- Adaptive Immune Responses are specific responses that generally occur over a longer period.
Take a look at the tree chart below as you continue reading below.
Please note that these charts are simplifications and do not represent the true complexity of the responses which often are combinations of specific and non specific responses.
Picture_Immune Response Types
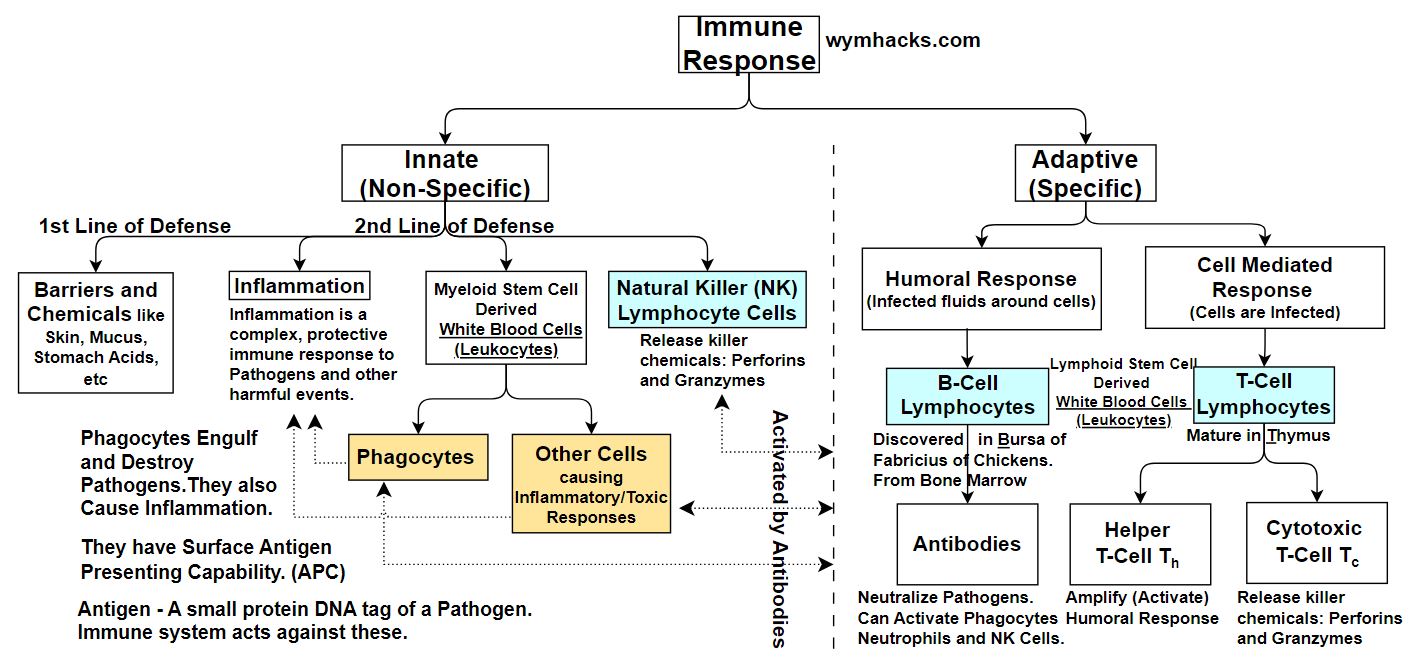
Innate Immune Response
The Innate (non specific) Immune Response has first and second lines of defense.
The first line involves the surface or near surface parts of our body and the second line kicks off when pathogens break through the first line. (we simplify a bit to define a specific demarcation which is a little arbitrary).
First Line of Innate Immune Defense
Skin or mucous membranes are the two main components of the 1st line of defense. Chemicals inside these barriers could also assist. The goal is to keep the bad things out.
Second Line of Innate Immune Defense
These responses kick in if pathogens have breached the first line of defense. Even internal cancer growths trigger this response.
Usually some kind of inflammatory response occurs in this stage (think heat, pain, redness, swelling). This involves blood vessels, immune cells, and chemicals.
White Blood Cells (WBCs) take part in this response.
- Some WBCs will engulf and destroy pathogens (like Macrophages) and
- others will kill them by chemical injection (Natural Killer or NK Cells) while
- others might create allergic reactions (Mast Cells, Basophils, Eosinophils etc.)
WBCs can act in a non specific way , reacting to any foreign pathogen, but also can act in very specific ways (and targeting specific pathogens).
In the chart above, we show Myeloid and Lymphoid derived WBCs as innate immune responders, but many of them also are integral parts of the Adaptive Immune System. The dotted lines are intended to convey this.
Adaptive Immune Response
Adaptive Immune Responses target specific pathogens. They are
- slower-acting,
- create immunological memory,
- target particular pathogens for elimination, and
- are adaptive, changing over time to combat new pathogens.
The big players here are WBCs called B-Cells and T-Cells.
- B-Cells are involved in combating pathogens outside of cells (Humoral Immune Response)
- T-Cells get involved when cells themselves have been infected (Cell Mediated Immune Response)
- Helper T-Cells are also integral in activating the Humoral Immune
Innate Immune Response
You should watch these two great videos on the Innate Immune System.
The Innate Immune Response system consists of two lines of defense.
- The First Line of Defense prevents pathogens (and other potentially harmful entities) from entering the body in the first place.
- It does this using physical or chemical barriers located near or at the surface of our body.
- The Second Line of Defense happens , for example, once pathogens have breached the first line (and other special situations like when combating cancer).
The picture below is a blow up of the left side of the full chart shown in the previous section. You can refer to this as you read the following descriptions of the Innate Immune System.
Picture_Innate Non Specific Immune Responses
First Line of Defense Physical Barrier Examples
- Skin, our largest organ, keeps harmful agents outside our body.
- Skin has a tough, relatively dry, and constantly shedding outer layer composed of tightly bound cells. This keeps many harmful organisms out.
- Its acidic environment keeps many bacteria from growing.
Mucous membranes, which can trap pathogens, line externally exposed openings and cavities.
These are found in our Respiratory System, Digestive System and Urogenital System (e.g. Urethra, Vagina).
Also, hair like Cilia trap and help expel pathogens.
First Line of Defense Chemical Barrier Examples
- e.g. Acids in the stomach, skin, and vagina
- e.g. Bacteria killing Enzymes like lysozyme in tears, saliva, and mucus
Second Line of Defense Examples
Second line defenses are innate cellular and chemical responses occurring after the first defense line is “breached”.
These responses are still considered non-specific in that they react to various pathogens in the same way. The first two items could really be considered first line of defense also but we wont get caught up in the semantics.
- e.g. Antimicrobial peptides and other substances on skin and other organs (called Defensins) : Chemicals that kill or inhibit the growth of microorganisms.
- e.g. Gut microbiome: These are beneficial and immune supporting bacteria in the gut.
Inflammatory Response: Involves blood vessels, immune cells, and chemicals.
- It’s the body’s natural response to injury, infection, or irritation.
- It’s a complex process involving various immune cells and chemicals (e.g. Histamines which Mast WBCs can emit).
- Inflammation Process: chemicals release, blood vessel dilation and increased permeability, swelling, and White Blood Cell involvement.
- Inflammation indicators: Redness, Swelling, Heat, Pain, Loss of function.
- The dilation and swelling allow protein rich fluids and WBCs to more easily reach the target area.
- The lymphatic system then cleans up excess fluids to be routed back to the blood stream.
White Blood Cell (WBC) Innate Responses
- WBCs in the Innate Response System can recognize pathogens (non-specifically) using Toll-Like Receptors or TLRs.
- TLRs detect Pathogen Associated Molecular Patterns (PAMPs).
- This triggers Phagocytosis as well as release of Cytokines and Chemokines which signal WBCs to fight the pathogen.
- Phagocytes: These WBCs engulf and destroy pathogens (e.g. Macrophages, Neutrophils, Dendritic Cells, etc.).
- Some WBCs destroy pathogens by chemical injection (e.g. Natural Killer Cells do this in a process called Apoptosis)
- Some WBCs produce Pyrogens which trigger the Hypothalamus to raise body temperature and produce fever.
- Fever causes higher temperature, speeding up cell repair and inhibiting the body from releasing nutrients beneficial to bacteria.
- Some WBCs provide an allergic response (e.g. Mast Cells, Basophils, Eosinophils).
Phagocytosis (a Bridge between Innate and Adaptive Responses)
Phagocytosis can be an Innate Immune process as it is triggered by non-specific Pathogen Associated Molecular Patterns (PAMPs).
But, Phagocytosis can also produce an Adaptive Immune Response specific to a singular pathogen.
Check out the picture below as you read on (sorry , I put teeth on my Pac-Man-like figure).
Picture_Phagocytosis and Antigen Production
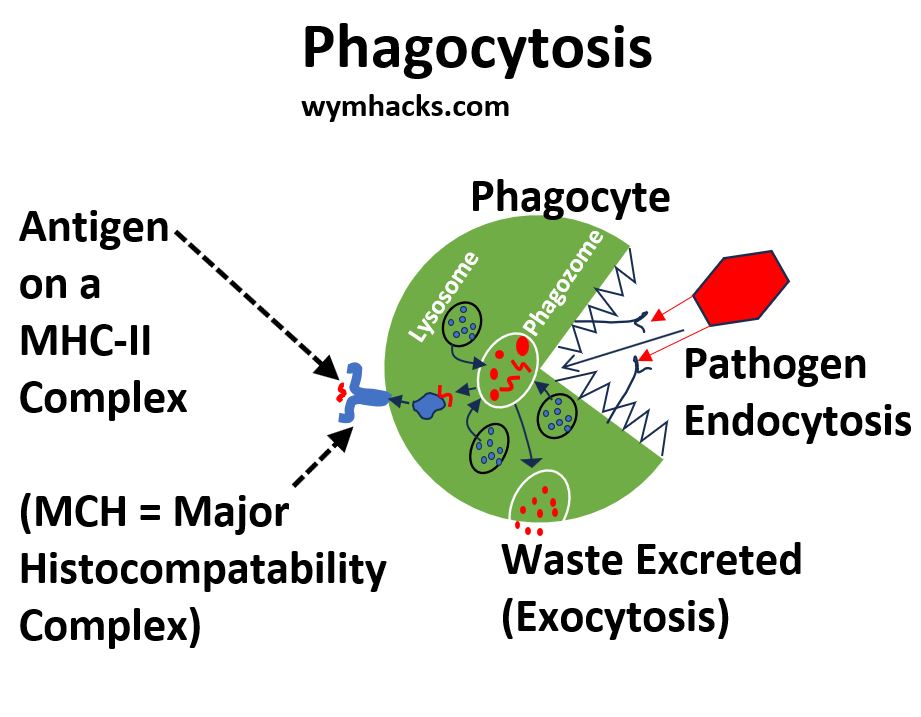
Phagocytes
- The “entity” is eventually swallowed (Endocytosis) and becomes a membrane bounded body inside the Phagocyte (called a Phagosome).
- Other bodies (Lysosomes) will attack and break down the contents of the Phagosome.
- Eventually the “digested” Phagosome drifts out to the surface and the contents are excreted as waste (Exocytosis).
Phagocytes Also Play a Part in the Adaptive Immune System
- Inside the Phagocyte, a protein complex called a Major Histocompatibility Complex II or MHC-II attaches itself to the Phagosome.
- It extracts one/some of the dissolved bits and then detaches and moves to the surface of the Phagocyte.
- The MHC-II sits on the surface and holds this marker of the bad actor. This is called an Antigen (typically a protein or peptide but not always).
- This kind of Phagocyte is called an Antigen Presenting Cell or APC.
Antigens are pathogen (and other bad actors) “markers or tags” and are critical players in Adaptive Immune Responses.
We will come back to this when we review B-Cells and T-Cells in the next section.
Adaptive Immune Response
Excellent References on the Adaptive Immune Response
You’ll get a solid firm foundational understanding of the the Adaptive Immune Response by watching the following videos.
- Khanacademy – Types of immune responses: Innate and adaptive, humoral vs. cell-mediated
- Khanacademy – B lymphocytes (B cells)
- Khanacademy – Professional Antigen Presenting Cells (APC) and MHC II complexes
- Khanacademy – Helper T cells
- Khanacademy – Cytotoxic T cells
- Khanacademy – Review of B cells, CD4+ T cells and CD8+ T cells
- Crash Course: Hank Green: Immune System, Part 2: Adaptive Humoral Response
- Crash Course: Hank Green: Immune System, Part 3: Adaptive Cell Mediated Response
Chart_Adaptive Immune Response
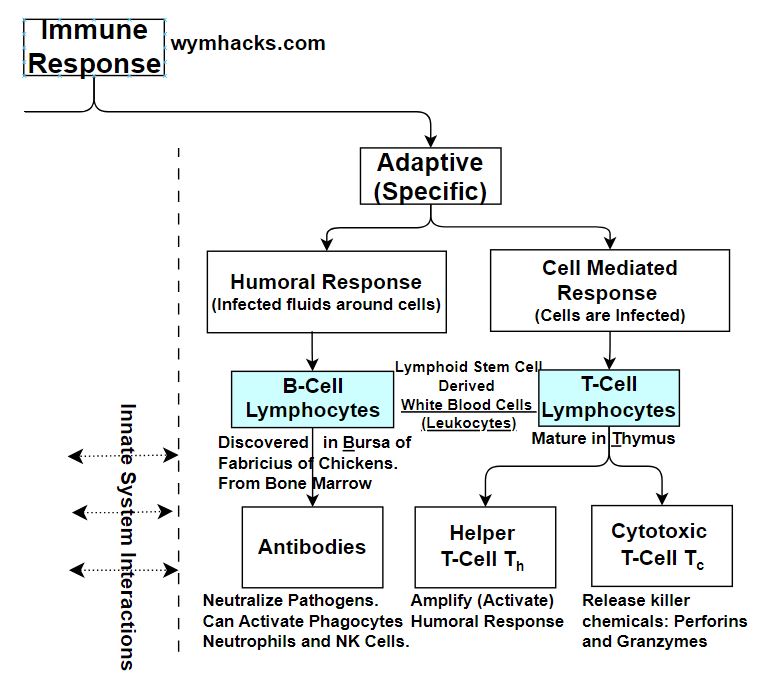
The Adaptive Immune Response system does two things differently than the Innate Response System:
- It targets and destroys specific bad actors (pathogens, cancerous cells, allergens etc.) but also
- produces “memory” White Blood Cells that are able to engage them more readily in future responses.
B-Cells , T-Cells and certain Phagocytes make this possible. So, let’s first describe these cells a little bit and then we can describe how they work together.
Antigen Presenting Cells (APC)
In the previous section we described how certain Phagocytic White Blood Cells (namely Dendritic Cells and Macrophages) can present Antigens on their surfaces.
As an Adaptive Immune System player, the Phagocyte destroys the bad actor but also presents a “marker” of it on its surface.
This marker is called an Antigen (usually a protein peptide chain) ,and it is presented on the surface attached to a protein called MHC-II (Major Histocompatibility Complex II).
This enables it to interact with T-Cells in a unique way.
T-Cells
T-Cells are made in Bone Marrow and they mature and develop in the Thymus, after which they are named.
- T-Cells are part of the body’s Adaptive Immune Response.
- They are involved in both extracellular (Humoral Response) and intracellular defenses (Cell Mediated Response).
- T-Helper (CD4) Cells interact with Antigens on B-Cells to activate B-cells. They also activate T-Cytotoxic cells.
- T- Cytotoxic (CD8) Cells release chemicals that kill pathogens that have infiltrated cells (e.g. cancer cells or cells infected with virus)
B-Cells
- Discovered in the Bursa of Fabricius of Chickens (where B in B-cells comes from).
- They are made (and also mature) in bone marrow.
- B-Cells are part of the body’s Adaptive Immune Response.
- They are Involved in extracellular defenses (Humoral Response).
- Attaching to a pathogen partially actives the B-Cell.
- B-Cells can engulf pathogens and present their Antigens on their surface.
- This Antigen Presenting capability allows T-Cells to activate them
- A fully activated B-Cell will produce Memory Cells and Effector Cells (Plasma Cells).
- Plasma Cells release Antibodies into the blood stream to combat pathogens.
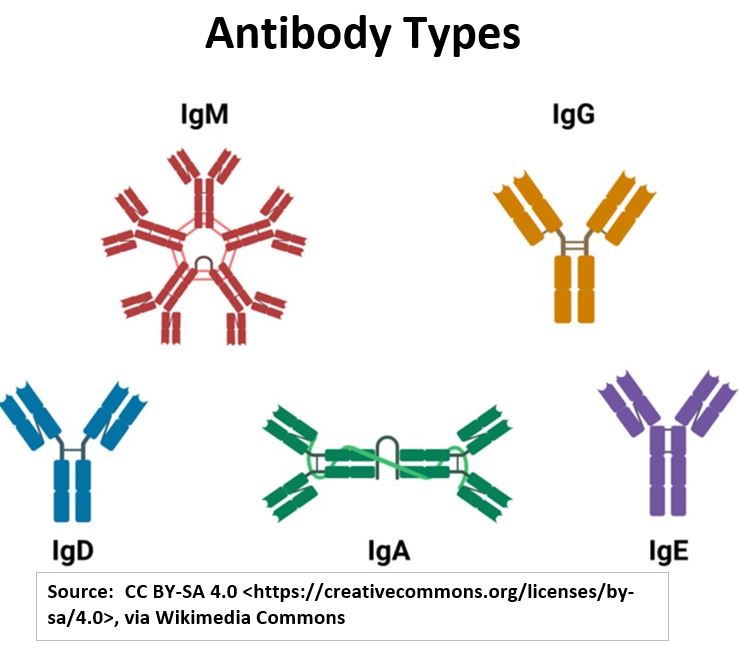
Antibodies
Antibodies are Y-shaped proteins produced by B-cells in response to Antigens. They are also called Immunoglobins.
- Antibodies are mainly produced in the Lymph Nodes.
- They are released into the Lymphatic system and eventually enter the bloodstream.
- Antibodies circulate in the bloodstream and bind specifically to Antigens, marking them for destruction by other immune cells.
Antibodies can
- neutralize pathogens,
- agglutinate them (make them stick together and thus neutralize them), or
- activate the complement system (proteins that lyse cells or improve Phagocytosis).
Antibody Structure and Functions:
- Y-shaped molecule: Consists of two identical heavy chains and two identical light chains.
- The “arms” of the Antibody are called the FAB Region (Fragment Antigen-Binding Region).
- Variable region of the FAB: Located at the tips of the Y, binds specifically to Antigens.
- “Variable” means structure and chemical composition (its amino acid sequence) varies greatly among different antibodies.
- The “stem” of the Antibody is called the Constant or FC Region (Fragment Crystallizable Region).
- The FC Region determines the Antibody’s class (IgM, IgG, IgD, IgA, IgE). Ig = Immunoglobin.
- So, while the FAB Region is involved in Antigen recognition and binding,
- the FC Region interacts with other immune cells and molecules to initiate a response.
Picture_Antibody Types
- Each Antibody has a unique Antigen-binding site (allowing for specific recognition of multitudinous bad actors).
- The binding site on the Antibody is called a Paratope.
- The binding site on the pathogen or other bad actor is called an Epitope.
The FC (stem) End of the Antibody Stimulates the Immune System into Action.
It activates Phagocytes into action against specific targets (Opsonization).
It activates the Complement System, a group of proteins that work together to destroy pathogens.
It activates Mast Cells to release Histamine and other inflammatory chemicals (causes allergic reactions also).
It activates Natural Killer Cells and Cytotoxic T-cells to recognize and kill target bad actors.
Picture_Antibody FAB and FC Regions
Ok, lets put all this together now.
B-Cell Activation in Adaptive Humoral Immune Responses
In a Humoral Adaptive Immune Response, B-Cells are stimulated to release Antibodies specifically targeting harmful entities existing outside of the body’s cells.
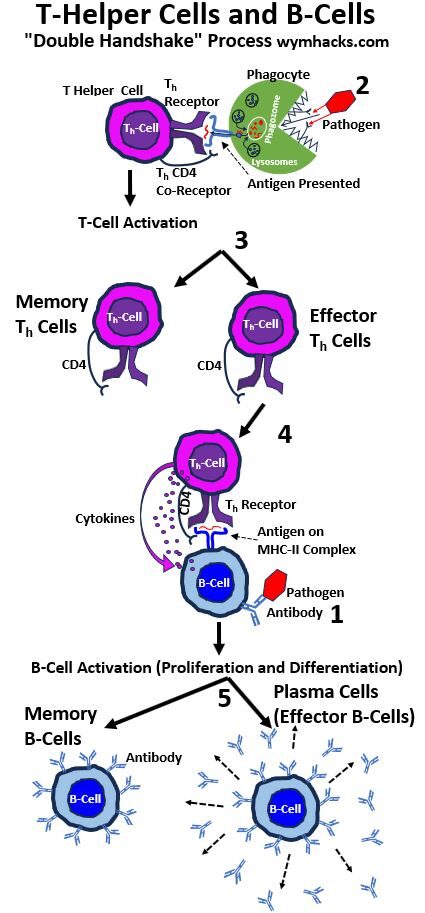
Look at the picture below as you read the following description of how B-Cells do this.
Picture_Helper T-Cells and Activation of B-Cells
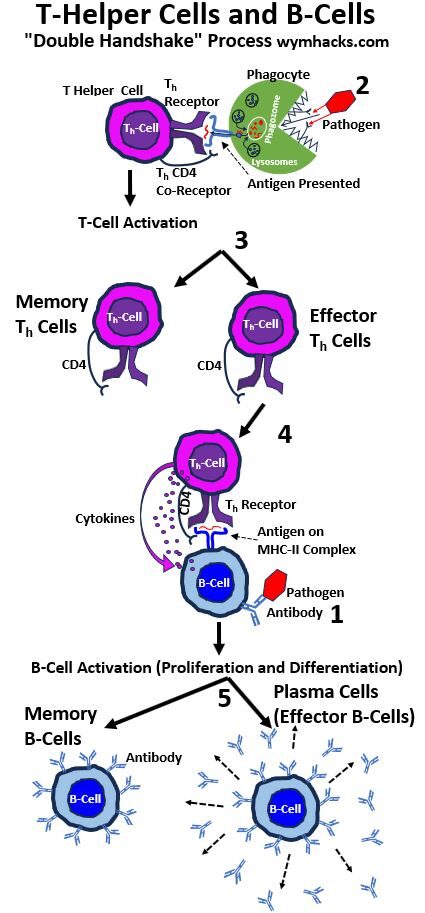
1a. B-Cells Produced With Specific Antibodies
B-Cells are produced in bone marrow in massive variety with specifically and uniquely structured Antibodies attached to their surfaces.
The variable stem ends of these Antibodies give each of them a unique binding structure for a specific pathogen.
The huge variety and diversity of B-Cell receptors with unique sites for unique pathogens (and their associated Antigens) increases the odds of the connection occurring. This diversity is generated through a process called V(D)J recombination.
Ultimately a B-Cell Surface Antibody will make the connection with a pathogen (Number 1 in the drawing above).
Note that , less commonly, The B-Cell can become activated and begin producing antibodies directly (step 1 to step 5 in the drawing) with no Helper T-Cell involvement (T-Cell-Independent).
In the following steps we focus on the more common T-Cell-Dependent path.
1b. B-Cells are Antigen Presenting Cells (APCs)
While the process is not exactly the same as how it occurs in Phagocytes (the other type of APCs), the pathogen attached to a B-Cell Antibody will eventually be engulfed and ultimately contribute an Antigen to a MHC-II complex.
Picture_The B-Cell is an Antigen Presenting Cell
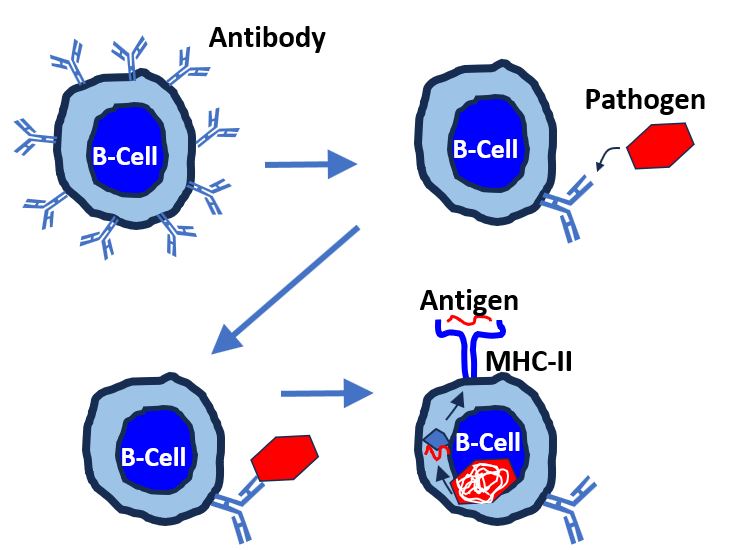
The Antigen laden MCH-II will rise and present itself on the surface of the B-Cell. It now is ready for activation by a Helper T-Cell.
2a. Antigen Presenting Phagocytes
Antigen-presenting cells (like Dendritic Cells or Macrophages) engulf the same pathogen, process its Antigens, and present them on their surface.
2b. Helper T-Cell Activation
Helper T-Cells recognize the presented Antigen and become activated.
3. Helper T-Cell Differentiation
The activated Helper T-Cells clone themselves and differentiate into Memory Helper T-Cells and Effector Helper T-Cells.
- Effector Helper T-Cells are short-lived cells that are direct actors. They produce Cytokines and Activate B-Cells.
- Memory Helper T-Cells are long-lived cells that remember past infections, allowing for a faster and stronger immune response when dealing with the same pathogen in the future.
4. Effector Helper T-Cells Activate B-Cells
B-Cells, already partially activated by attaching to the same pathogen, are now totally activated by the Effector T-Cells. Remember, the Effector Helper T-Cells are only acting on this singular specific pathogen.
The Effector Helper T-Cells also release Cytokines into the B-Cell further activating it into the Antibody production.
5. Full B-Cell Activation
The B-Cell is now fully activated by having two “things” happen to it
- The B-Cell was initially activated by the Pathogen.
- The B-Cell was finally activated by a specialized Effector Helper T-Cell (through Cytokines and attachment to the Antigen on the MHC-II complex).
The B-Cell now clones and differentiates into Memory B-Cells and Effector B-Cells (also called Plasma Cells…has nothing to do with Blood Plasma).
Memory B-Cells are specialized for any future engagement with the same pathogen.
The Plasma B-Cells produce large quantities of Antibodies specific to the original pathogen.
The Antibodies ultimately get to the blood where they “engage the enemy” as needed.
Shit, that’s pretty cool.
Now, the above was all about a Humoral (not in the cell) Adaptive Immune Response; spearheaded by B-Cells and enabled by T-Cells.
But how does the Immune System battle infected or cancerous cells? We want to discuss this Cell Mediated Immune Response next.
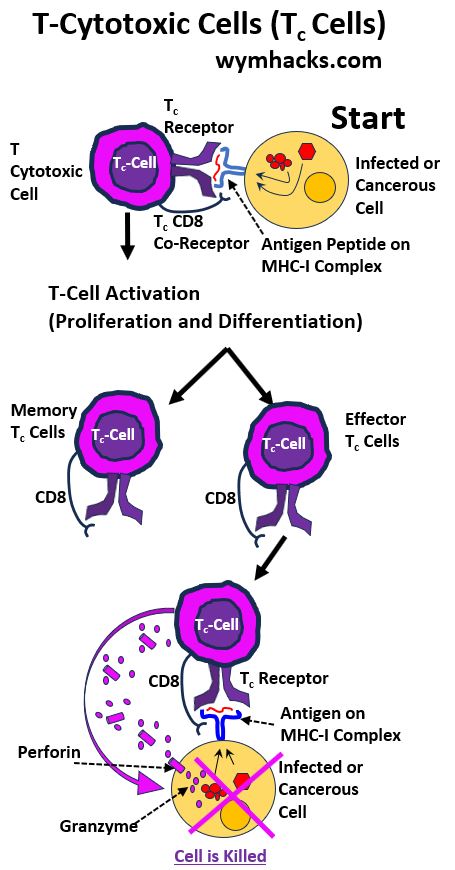
The Roll of T-Cells in Adaptive Cell Mediated Immune Responses
When the Immune System acts on an infected cell, we call this a Cell Mediated Immune Response.
We saw how Helper T-Cells stimulate B-Cells to release Antibodies to attack pathogens outside of cells (Humoral Immune Response).
Another Lymphocytic White Blood Cell called a Cytotoxic T-Cell helps battle infected and cancerous cells (Cell Mediated Immune Response).
As I explain how, you can follow along with the picture below.
Picture_Cytotoxic T Cell Activation
Let’s say some of our body cells are infected with a virus (or a cancer). How does our Immune System deal with these kinds of attacks?
1. Infected Cell Produces an Antigen on an MHC-I Complex on its Surface
The infected cell itself will present an Antigen on its surface but now it’s embedded in an MHC-I protein complex. This cell has effectively marked itself for death.
T-Cells (just like B-Cells and Antibodies) undergo a process called V(D)J recombination during their development, which generates a vast array of unique T cell receptors (TCRs).
This allows Cytotoxic T-Cells to find and bind with specific Antigens presented on MHC-I complexes.
2. Cytotoxic T-Cell Activation
A Cytotoxic T-Cell binds to the Infected Cell and Becomes Activated.
The activated Cytotoxic T-Cell begins cloning and differentiating into Memory and Effector Cytotoxic T-Cells (Just as we saw before with Helper T-Cells and B-Cells).
Memory Cytotoxic T-Cells are specialized for any future engagement with the same infected or cancerous cell.
3. Effector Cytotoxic T-Cells Kill the Infected or Cancerous Cell
Effector Cytotoxic T-Cells begin emitting killer chemicals called Perforin and Granzyme.
The Perforin perforates the cell and the Granzyme chemicals kill it. (process called Apoptosis).
Vaccinations
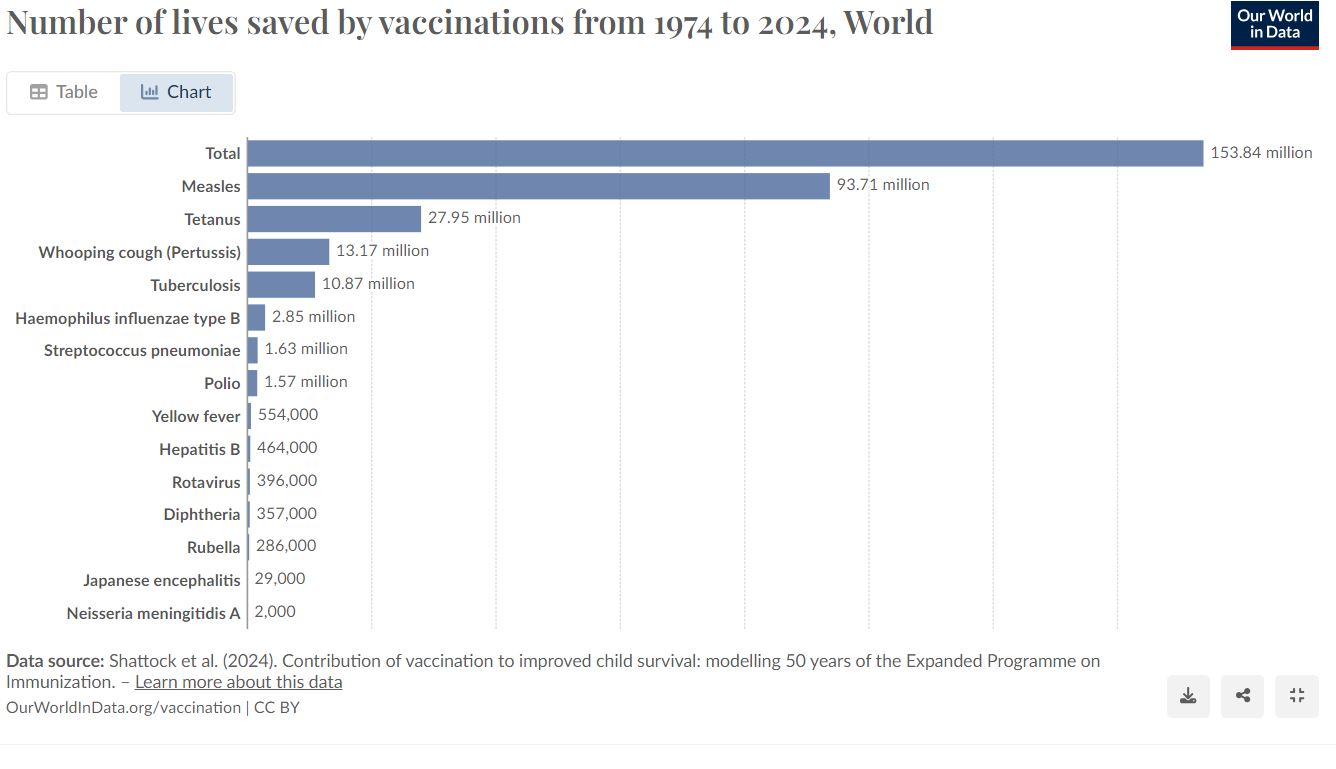
Vaccinations protect you against harmful diseases, before you come into contact with them.
According to the WHO:
- “Vaccines train your Immune System to create antibodies, just as it does when it’s exposed to a disease.
- However, because vaccines contain only killed or weakened forms of germs like viruses or bacteria, they do not cause the disease or put you at risk of its complications.”
- “Global immunization efforts have saved at least 154 million lives over the past 50 years”
Picture_Number of Lives Saved by Vaccinations (1974-2024)
Early History
1400s to 1700s
- From at least the 15th Century (but perhaps much earlier into BCE) healthy people were intentionally exposed to Smallpox in order to prevent the illness.
- Practice coined as “Variolation” in the 18th century (from Latin “variola,” which means “spotted” or “pimpled”).
- (1721) Lady Mary Wortley Montagu introduced smallpox inoculation to Europe (as she had observed the practice in Turkey).
1796
- In May – July 1796, English physician Edward Jenner Makes the First Vaccination.
- 8-year-old James Phipps is inoculated with pus from a cowpox sore (on the hand of a milkmaid).
- Phipps made a full recovery.
- Phipps then is inoculated with matter from a human Smallpox sore and Phipps is immune to it.
- Huge discovery: A much milder disease (cowpox) with significantly less risk is used to provide immunity to a much more dangerous disease (Smallpox).
Picture_Milkmaid Sarah Nelmes’s Hand
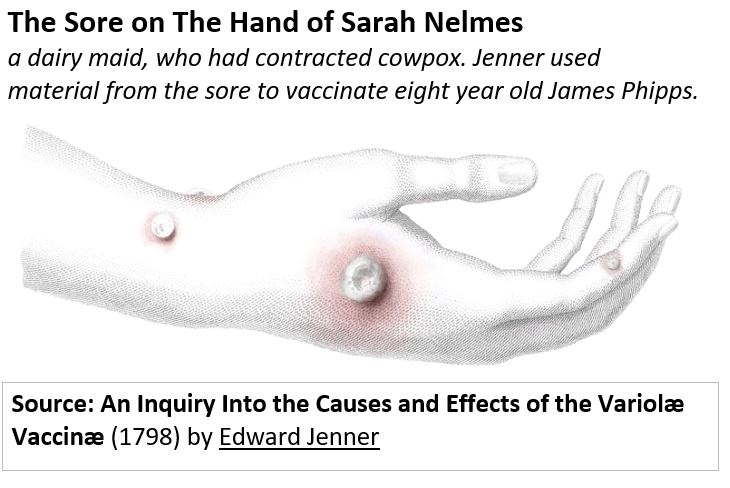
- Thus, Phipps becomes the first human to be vaccinated against Smallpox.
- Jenner coined the word “Vaccination” which
- is a combination of the Latin word for cow (vacca) , and cowpox (vaccinia).
- Vaccination differs from the much riskier Variolation in which a person is directly exposed to the pathogen.
How Jefferson and Franklin Helped End Smallpox in America
- Excerpts of a letter from Jefferson to Jenner: “… I avail myself of this occasion of rendering you a portion of the tribute of gratitude due to you from the whole human family. Medicine has never before produced any single improvement of such utility… You have erased from the calendar of human afflictions one of its greatest. Yours is the comfortable reflection that mankind can never forget that you have lived. Future nations will know by history only that the loathsome small-pox has existed and by you has been extirpated. Accept my fervent wishes for your health and happiness and assurances of the greatest respect and consideration.”
- Wouldn’t you love to get a letter like that?
Key Viruses and their Vaccination Developers
Smallpox / First Vaccination by Edward Jenner / 1796
- WHO – History-of-smallpox-vaccination
- Smallpox killed 30% of those who contacted it.
- It destroyed a large % of Aztec Peoples and Indigenous Americans.
- Smallpox has killed more than 300 million people since 1900 alone.
- Smallpox remains the only human disease to have been eradicated. (took till 1980 to do it)
List of Diseases that have Vaccinations
- Adenovirus
- Anthrax
- Chickenpox (varicella)
Cholera
- COVID-19 (corona virus)
- Dengue
- Diphtheria
- Flu (influenza)
- Hepatitis A
- Hepatitis B
- Hepatitus E
- Hib (Haemophilus influenzae type b)
- HPV (human papillomavirus)
Influenza
- Japanese Encephalitis (JE)
Malaria
Measles
- Meningococcal meningitis
- Mpox (Formerly Monkeypox)
- Mumps
- Pertussis (whooping cough)
- Pneumococcal disease
- Polio
- Rabies
- Rotavirus
- RSV (respiratory syncytial virus)
- Rubella (German Measles)
- Shingles (herpes zoster)
Smallpox
- Tetanus (lockjaw)
- Tick-borne encephalitis
Tuberculosis
- Typhoid
- Yellow fever
A Cellular View of How Vaccinations Work
Vaccinations Trigger a Humoral Adaptive Immune Response
The “part or piece” of a pathogen used in a Vaccination can assume various forms:
- a weakened or killed form of the microbe itself,
- an inactivated version of its toxins,
- or a protein from the surface of the microbe.
This triggers the typical Humoral Adaptive Immune Response resulting in the production of Antibodies.
Recall the picture below from the Adaptive Immune Response Section. The pathogen shown in 1 and 2 in this picture would now be the vaccination piece and not the full natural form of the pathogen.
The remaining parts of the process would be the same, resulting in Antibody producing B-Cells.
Note: It’s possible for B-Cell Antibody production without the help of Helper T-Cells but this is less common.
Picture_Helper T-Cells and B-Cells
The vaccination concept is a brilliant one i.e. “the introduction of a milder form of the pathogen such that the body can begin to develop immunity.”
Without the vaccine, a person’s first exposure to the actual pathogen might prove very harmful or fatal. This has proven to be much safer and more effective than the earlier practice of Variolation.
Immune System Disorders
A lot of things can go wrong with our Immune Systems.
Primary Immune Deficiency (Immunodeficiency at Birth)
Sometimes people are born with weakened immune systems. Examples include:
- Severe Combined Immunodeficiency (SCID) ;sometimes called “bubble boy disease”.
- Others:
- CVID
- X-linked Agammaglobulinemia
- Chronic Granulomatous Disease (CGD)
- Wiskott-Aldrich Syndrome (WAS)
Acquired Immune Deficiency (Immunodeficiency after Birth)
Immune Systems can also be weakened after birth due to infections, medications, or other factors. Examples include:
- Acquired Immunodeficiency Syndrome (AIDS) caused by the Human Immunodeficiency Virus (HIV)
- Immunosuppression due to medications like Corticosteroids, chemotherapy, and immunosuppressants used in organ transplantation
- Deficiencies caused by infections like flu virus, mono (mononucleosis) and measles
- Problems caused by smoking, alcohol, and poor nutrition (not always your choice)
- Immune Deficiencies caused by chronic (long term) stress
Autoimmune Immune Disorders
In Autoimmune Disorders, the body generates an immune response against itself (it attacks itself). Examples are:
- Psoriatic arthritis.
- Rheumatoid arthritis (RA).
- Sjögren’s syndrome.
- Systemic lupus erythematosus (Lupus, SLE).
- Crohn’s disease.
- Celiac disease.
- Ulcerative colitis.
- Graves’ disease.
- Hashimoto’s thyroiditis.
- Addison’s disease.
- Dermatomyositis.
- Psoriasis.
- Chronic inflammatory demyelinating polyneuropathy (CIDP).
- Guillain-Barre syndrome.
- Multiple sclerosis (MS).
- Myasthenia gravis.
- Type 1 diabetes.
- Pernicious anemia.
- Vasculitis.
Excessive Immune Responses
The body over-reacts to often harmless foreign Antigens and damages normal tissues (an allergic reaction).
- Asthma: (coughing, wheezing, and trouble breathing). Asthma can be triggered by dust and pollen allergens or even tobacco smoke.
- Eczema: Some allergens can cause Atopic Dermatitis (itchy rash).
- Allergic Rhinitis (Hay Fever): Allergens like dust, pet dander, pollens or molds etc. can aggravate your nasal passages (causing sneezing, runny nose, swelling etc.)
Immune Health
Our immune health is a multivariable and complicated process which intertwines with our other body functions. And, our own specific genetics add another layer of complexity.
Therefore, absolutely proving (i.e. conducting valid studies) the cause and effect of any particular diet or exercise on a benefit is very difficult.
So, you should be very leery if you hear or see someone touting some magic “elixir” or behavior that directly correlates to some stated benefit.
My general learning from all my readings and video viewings is that there is no shortcut to improving your health.
You know what you have to do (see my articles : Diet and Fitness Plan and Nutritional Guidelines with Supplement Comments)
- Get regular checkups so you can stay ahead of any issues.
- Try to maintain a reasonable body weight (defined by BMI for example).
- Exercise regularly and mix in both aerobic and strength training routines.
- And maybe try a few other things to chill you out (stretch, meditate, take short or long walks , etc.).
- Follow the Dietary Guidelines for Americans.
- Supplement nutrients that you otherwise are not getting from your normal diet.
- Don’t smoke and try to not drink too much alcohol.
In the following sections, I list nutrients and best practices that most people agree will have a positive impact on your immune health. Not surprisingly these things will contribute to an improved overall health as well. Links to the References (e.g. Ref 1) are listed at the end of this section on Immune Health.
You’re Getting Older
As you age, you will be more susceptible to disease and infection.
- Are you making sure you are adequately monitoring your body?
- Are you up to date on your vaccines?
- Are you getting regular medical checkups?
- Are your lifestyle habits (exercise, what you eat and drink and how much you sleep) consistent with your desire for a long and pain free life?
(Ref 7) “As we age, our internal organs may become less efficient; immune-related organs like the thymus or bone marrow produce less immune cells needed to fight off infections. Aging is sometimes associated with micronutrient deficiencies, which may worsen a declining immune function.”
Avoid Getting Infected
Ref 3; Ref 5;Ref 7, Ref 9
- (Ref 3) “Wash your hands for 20 seconds, don’t touch your face and take social distancing seriously when around anyone who seems sick”
- Wash Hands (Ref 7; “when coming in from outdoors, before and after preparing and eating food, after using the toilet, after coughing or blowing your nose”).
- Cook food sufficiently
Get Regular Medical Screenings
Ref 6; Ref 9;
- (Ref 9) “Get regular medical screening tests for people in your age group and risk category.”
- For guys (prostate check, colonoscopies) and for women (breast checks, colonoscopies)
Don’t Smoke
Ref 1; Ref 4; Ref 5;Ref 6; Ref 7; Ref 9
- (Ref 1) “Smoking can make the body less successful at fighting disease. Smoking increases the risk for Immune System problems, including rheumatoid arthritis.“
- (Ref 4) “Smoking exacerbates pathogenic immune responses and/or reduces immune defenses.”
Exercise (Including Meditation and Stretching)
Ref 1; Ref 3; Ref 4; Ref 5;Ref 6; Ref 7; Ref 8; Ref 9; Ref 11; Ref 12; Ref 14
Exercise_(References 1 – 11)
- (Ref 1) “Emerging research also suggests that physical activity may potentially benefit immunity.”
- (Ref 1) “..being physically active may help lower your chances of dying from the flu or pneumonia.”
- (Ref 4) “Exercise changes immune regulation by affecting cells and has anti-inflammatory effects.”
- (Ref 8) Reduces Inflammation
- (Ref 9, Ref 11); Weekly Target: 2 strength training sessions and 150 minutes of moderate cardiovascular activity
- (Ref 11); “Moderate cardiovascular exercise can increase the activity of virus-killing cells. This includes White Blood Cells and antibodies.
- (Ref 11); “Muscle tissue preserved from strength training secretes anti-inflammatory substances called myokines.”
Exercise_(Reference 14)
- (Ref 14) Exercise helps decrease your chances of developing heart disease and keeps your bones healthy and strong,
- (Ref 14) Flushes bacteria out of the lungs, reducing chance of getting a cold, flu, or other illness.
- (Ref 14) White Blood Cell antibodies circulate more rapidly, thus detecting illnesses earlier than normal.
- (Ref 14) Body temperature rise might fight infections better (similar to when you have a fever)
- (Ref 14) Slows down the release of stress hormones, some of which increase the chance of illness.
Sleep (7-9 hours/day)
Ref 1; Ref 4; Ref 5;Ref 6; Ref 7; Ref 9; Ref 11; Ref 12
- (Ref 4) “Sleep loss
- reduces natural killer cell activity, which increases the risk for cancer and viral infections;
- generates production of inflammatory Cytokines, which increases the risk for cardiovascular and metabolic disorders;
- and reduces production of antibodies, which increases the risk for infections.
- (Ref 11, Ref 13) Sleep deprivation might reduce the release of Cytokines which help fight off infection.
Maintain a Healthy Weight
Ref 1; Ref 5;Ref 6; Ref 7; Ref 9
Are you in a healthy weight range? You can use information in my Diet and Fitness Plan to estimate your Body Mass Index or BMI.
- (Ref 1) “Obesity, defined as a body mass index (BMI) of 30 or more in adults, is linked to impaired immune functions.”
- (Ref 1) “Obesity may also lower vaccine effectiveness for diseases like influenza, hepatitis B, and tetanus.”
- (Ref 7) “Obesity is associated with low-grade chronic inflammation.
- Fat tissue produces Adipocytokines that can promote inflammatory processes.
- Research is early, but obesity has also been identified as an independent risk factor for the influenza virus, possibly due to the impaired function of T-cells, a type of White Blood Cell. “
Stay Hydrated
- (Ref 2) “Water helps your body produce lymph, which carries White Blood Cells and other Immune System cells,”.
- (Ref 2) “…try eating more hydrating foods, such as cucumbers, celery and watermelon.”
Control your Blood Pressure
Ref 9
- Your regular yearly (at least) medical checkups should include a blood pressure check.
- If it’s too high (discuss with your doctor), you guys need to come up with a plan to manage it. Avoid being a victim of this “silent killer”.
According to the World Heart Federation (accessed 8/18/2024):
- “Hypertension is the number one risk factor for death globally, affecting more than 1 billion people.
- It accounts for about half of all heart disease and stroke-related deaths worldwide.
- Hypertension does not cause any symptoms on its own, which is why it’s often referred to as “the silent killer”.
A high blood pressure patient probably has some or all of the following: inflammation, endothelial dysfunction, oxidative stress, and altered immune cell function.
But are these symptoms or causes?
Recent studies have suggested that inflammation caused by the Immune System ultimately results in chronic hypertension. This is an ongoing research area.
Drink Alcohol in Moderation
Ref 1; Ref 4; Ref 5;Ref 6; Ref 7; Ref 9;
(Ref 4) Alcohol disrupts immune pathways, contributes to organ damage, and impedes recovery from tissue injury.
Diet (Follow the American Dietary Guidelines)
Ref 1; Ref 3; Ref 4; Ref 5;Ref 6; Ref 7; Ref 11; Ref 12; Ref 15
Follow the American Dietary Guidelines. Supplement to fill the gaps but try to get as much as possible through food.
You can use the guidelines as a baseline from which to begin. You can tweak according to your own experimentation and feedback from your body.
Diet_(Refences 1 – 4)
- (Ref 1) “Eating well means emphasizing plenty of fruits and vegetables, lean protein, whole grains, and fat–free or low–fat milk and milk products.”
- (Ref 1) “Eating well also means limiting saturated fats, salt, and added sugars.”
- (Ref 3) “Choosing whole, unprocessed foods does wonders for overall health.”
- (Ref 3) Garlic (Allicin) can boost the Immune System.
- (Ref 3) Prebiotics: Robust gut bacteria protect us against infection. Keep those bacteria healthy with prebiotics that contain fiber, specifically inulin fiber.”
- (Ref 3) Vitamin C-rich foods: Vitamin C is known to boost immunity.
- (Ref 3) Antioxidants: “Colorful fruits and vegetables including berries, carrots and spinach have antioxidants that protect you against oxidative stress, which translates to a stronger Immune System.”
- (Ref 4) “Eat as many fresh fruits and vegetables as you can, every day.” – For Zinc and Vitamin A for example.
- (Ref 4) ” The fiber from fruit and vegetables can help your gut’s microbiome produce important compounds for a healthy Immune System.”
Diet_(Refence 7)
- (Ref 7) “Eat a balanced diet with whole fruits, vegetables, lean proteins, whole grains, and plenty of water. A Mediterranean Diet is one option that includes these types of foods”
- (Ref 7) “… a Western diet high in refined sugar and red meat and low in fruits and vegetables can promote disturbances in healthy intestinal microorganisms, resulting in chronic inflammation of the gut, and associated suppressed immunity.”
- (Ref 7) “If a balanced diet is not readily accessible, taking a multivitamin containing the RDA for several nutrients may be used.”
- (Ref 7) “Certain dietary patterns may better prepare the body for microbial attacks and excess inflammation, but it is unlikely that individual foods offer special protection.”
- (Ref 7) Vitamin C, vitamin D, zinc, selenium, Iron, and Protein (e.g. glutamine) are identified as critical for the growth and function of immune cells
- (Ref 7) “The gut is a major site of immune activity and the production of antimicrobial proteins. The diet plays a large role in determining what kinds of microbes live in our intestines.”
- (Ref 7) “A high-fiber plant-rich diet with plenty of fruits, vegetables, whole grains, and legumes appear to support the growth and maintenance of beneficial microbes.”
- (Ref 7) Prebiotics break down fibers into short chain fatty acids, which have been shown to stimulate immune cell activity.
- (Ref 7) A diet containing probiotic (gut helpful bacteria) and prebiotic foods (feed and maintain these bacteria) may be beneficial.
Diet_(Refences 11 -15 )
- (Ref 11) “Minimally processed whole foods — especially whole plant foods — may reduce inflammation by improving gut health.”
- (Ref 15) “Consuming adequate amounts of several vitamins and minerals—including vitamin A, vitamin C, vitamin D, vitamin E, selenium, and zinc—is important for proper immune function,…”
- (Ref 15) “and clinical deficiencies of these nutrients weaken immunity and can increase susceptibility to infections”
Vitamins and Minerals
Vitamin_A
- (Ref 15) “Vitamin A plays a critical role in vision and growth. It is also required for the formation and maintenance of epithelial tissue and the differentiation, maturation, and function of Macrophages and other cells of the innate Immune System”
- (Ref 15) “Vitamin A’s impact on adaptive immunity is less clear, but it is involved in the maturation of CD4+ T-Cells, the function of B-cells, and the regulation of inflammatory Cytokines”
- (Ref 15) “Vitamin A deficiency is associated with increased susceptibility to infections, altered immune responses, and impairment in the ability of epithelial tissue to act as a barrier to pathogens”
Vitamin_B6
- (Ref 2) “B6 is vital to supporting biochemical reactions in your Immune System. One of its major roles is in producing White Blood Cells and T-cells.”
Vitamin_C
Ref 2; Ref 7; Ref 11; Ref 15
- (Ref 2) “Vitamin C acts as an antioxidant, meaning it can protect your body from toxins that cause inflammation in your body.”
- (Ref 11) Maybe help with cold recovery.
- (Ref 15) “Vitamin C plays an important role in both innate and adaptive immunity, probably because of its antioxidant effects, antimicrobial and antiviral actions, and effects on Immune System modulators.”
- (Ref 15) “Vitamin C helps maintain epithelial integrity, enhance the differentiation and proliferation of B- Cells and T-Cells, enhance Phagocytosis, normalize Cytokine production, and decrease Histamine levels”
- (Ref 15) “It might also inhibit viral replication””
- (Ref 15) “Vitamin C deficiency impairs immune function and increases susceptibility to infections”
Vitamin_D
Ref 3, Ref 7; Ref 11; Ref 15
- (Ref 3) “…a deficiency may increase your susceptibility to infection,.. Get outside for fresh air and sunshine, but also consider taking a daily supplement of 1,000 to 2,000 IUs of vitamin D.”
- (Ref 11) Make sure you are getting the RDA for Vitamin D. Helps safeguard adaptive immune cells that decline with age. RDA (600 IU <70 yrs age and 800 IU for >70 yrs age.)
- (Ref 15) “Vitamin D appears to lower viral replication rates, suppress inflammation, and increase levels of T-regulatory cells and their activity.”
- (Ref 15) “In addition, almost all immune cells (e.g., B Lymphocytes and T Lymphocytes) express the vitamin D receptor, and some immune cells (e.g., Macrophages and Dendritic Cells) can convert 25(OH)D to the active 1,25(OH)2D form. These capabilities suggest that vitamin D can modulate both innate and adaptive immune responses”
Vitamin_E
Ref 2;Ref 15
- (Ref 2) “Vitamin E is a powerful antioxidant that helps your body fight off infection… it helps keep your T-cells working at peak performance.”
- (Ref 15) “… plays an important role in immune function by helping maintain cell membrane integrity and epithelial barriers and by enhancing Antibody production, Lymphocyte proliferation, and natural killer cell activity.”
- (Ref 15) “Vitamin E also limits inflammation by inhibiting the production of proinflammatory Cytokines”.
- (Ref 15) “Human and animal studies suggest that vitamin E deficiency impairs humoral and cell-mediated immunity, is associated with reduced natural killer cell activity, and increases susceptibility to infections.”
Selenium
Ref 2; Ref 7; Ref 15
- Selenium, Selenoproteins and Viral Infection;
- (Ref 2) “Dietary selenium is a one-two punch for keeping you healthy. Researchers say it not only activates your Immune System when there’s a threat, but it also tells your Immune System when to pump the brakes.
- (Ref 2) “…it can keep your Immune System from going overboard, protecting you from chronic inflammation and autoimmune diseases, like rheumatoid arthritis, Crohn’s disease and psoriasis.
- (Ref 15) “Human and animal studies suggest that selenium helps support both the innate and adaptive Immune Systems through its role in T-cell maturation and function and in natural killer cell activity.”
- (Ref 15) “It may also reduce the risk of infections.”
- (Ref 15) “As a component of enzymes that have antioxidant activities, selenium might help reduce the systemic inflammatory response that can lead to ARDS and organ failure”
- (Ref 15) “Low selenium status in humans has been associated with lower natural killer cell activity, increased risk of some bacterial infections, and increased virulence of certain viruses, including hepatitis B and C”
Zinc
Ref 2, Ref 4; Ref 7; Ref 11; Ref 15
Zinc_(References 2 – 11)
- (Ref 2) “Zinc is an anti-inflammatory and antioxidant. Researchers call it the “gatekeeper” of your Immune System because it’s responsible for making all your immune cells function properly.”
- (Ref 4) “Taking Zinc supplements at the beginning of a respiratory infection can reduce the severity and duration of symptoms. Ask your doctor to recommend brands and appropriate dose for you.”
- (Ref 11) May help with cold recovery.
Zinc_(Reference 15)
- (Ref 15) “Zinc is involved in numerous aspects of cellular metabolism. It is necessary for the catalytic activity of approximately 100 enzymes and it plays a role in many body processes, including both the innate and adaptive Immune Systems”
- (Ref 15) “Zinc also has antiviral and anti-inflammatory properties, and it helps maintain the integrity of tissue barriers, such as the respiratory epithelia.”
- (Ref 15) “Zinc deficiency adversely affects immune function by impairing the formation, activation, and maturation of Lymphocytes.”
- (Ref 15) “Zinc deficiency decreases ratios of helper to suppressor T-Cells, production of interleukin-2, and activity of natural killer cells and cytotoxic T-Cells”
- (Ref 15) “Zinc deficiency is associated with elevated levels of proinflammatory mediators. These effects on immune response probably increase susceptibility to infections [163] and inflammatory diseases, especially those affecting the lungs.”
Extra Dosages of Vitamins
- (Ref 9) “So far, there is no evidence that taking extra amounts of any vitamin will improve your Immune System or protect you if you don’t have micronutrient deficiencies.
- (Ref 9) “However, older people, who are more likely to have such deficiencies, should discuss this question with a physician who is well versed in geriatric nutrition.”
Botanicals
Andrographis
- (Ref 15) “The active constituents of andrographis are believed to be andrographolide and related compounds, which are diterpene lactones that might have antiviral, anti-inflammatory, and immune-stimulating effects”
Echinacea
- (Ref 15) “Echinacea might have antibacterial activities, stimulate monocytes and natural killer cells, and inhibit virus binding to host cells. It might also reduce inflammation by inhibiting inflammatory Cytokines.”
Elderberry (European Elder)
- (Ref 15) “Elderberry contains many compounds—including anthocyanins, flavonols, and phenolic acids—that might have anti-inflammatory, antiviral, antimicrobial, and immune-stimulating effects”
Garlic
- (Ref 15) “Researchers have studied garlic mainly to determine whether it lowers blood pressure and cholesterol levels, but it might also have antiviral properties”
Ginseng
- (Ref 15) “Animal and laboratory studies suggest that ginseng stimulates B-Lymphocyte proliferation and increases production of some interleukins and interferon-gamma [251]; these Cytokines affect immune activation and modulation.
- (Ref 15) “Ginseng might also inhibit virus replication and have anti-inflammatory activity.”
Tea and tea catechins
- (Ref 15) “Tea is one of the richest sources of catechins, which are polyphenolic flavonoids, especially epigallocatechin gallate (EGCG)”
- (Ref 15) “Studies are evaluating the potential health benefits of EGCG and other catechins, including their ability to modulate the Immune System and their anti-inflammatory and antimicrobial properties.”
- (Ref 15) “Laboratory studies suggest that catechins might also have antiviral effects against the influenza A and B viruses”
Other Nutrients
Glutamine
- (Ref 15) “In the Immune System, glutamine is involved in Lymphocyte proliferation and Cytokine production as well as Macrophage and Neutrophil function [286]. Low glutamine levels are associated with poor immunologic function and an increased risk of mortality in patients in the ICU”
N-acetylcysteine and Glutathione
- (Ref 15) “N-acetylcysteine (NAC) is a derivative of the amino acid cysteine. NAC is an antioxidant that has mucolytic activity, so it helps reduce respiratory mucus levels.”
- (Ref15) “NAC might improve Immune System function and suppress viral replication”
- (Ref 15) “NAC also appears to decrease levels of interleukin-6 and have other anti-inflammatory effects”
- (Ref 15) “Laboratory and animal studies suggest that glutathione has antioxidant activity and appears to have antiviral and antimicrobial effects and enhance natural killer cell and neutrophil activity”.
- (Ref 15) “Glutathione may also have anti-inflammatory effects via altered Cytokine expression.”
- (Ref 15) “Adequate glutathione levels are needed for optimal innate and adaptive Immune System function, including proper T-cell activation and differentiation”
Omega 3 Fatty Acids
- (Ref 15) “Higher intakes and higher blood levels of EPA and DHA are associated with lower levels of inflammatory Cytokines, such as Interleukin-1 and Interleukin-6”.
- (Ref 15) “Immune system cells can easily incorporate EPA and DHA, which might also affect immune function by upregulating the activity of Macrophages, Neutrophils, T-Cells, B-Cells, natural killer cells, and other immune cells. “
- (Ref 15) “In addition, omega-3s may have antimicrobial and antiviral effects.”
Probiotics
- (Ref 15) “Probiotics are live microorganisms that confer a health benefit on the host when administered in adequate amounts.”
- (Ref 15) Probiotics act mainly in the gastrointestinal tract [7]. They might improve immune function in several ways, including by enhancing gut barrier function, increasing immunoglobulin production, inhibiting viral replication, and enhancing the Phagocytic activity of White Blood Cells.”
- (Ref 15) Some studies suggest that probiotics increase levels of Natural Killer Cells, Lymphocytes, and monocytes and that they decrease levels of proinflammatory Cytokines, but other studies do not.”
Manage/Reduce Stress
Ref 3; Ref 4; Ref 5;Ref 6; Ref 7 ; Ref 12
- Mayclinic.org – Chronic stress puts your health at risk
- (Ref 3) Sleep, Meditate, Exercise (ideally 30 minutes a day; strength building plus cardio)
- (Ref 4) Psychological and physical stress weakens parts of your Immune System. Example: Shingles flares up when people are experiencing chronic stress.
- (Ref 4) “Stress can also cause “patrols” in your Immune System—certain cells that tell the Immune System to wind down an attack—to fail. When this happens, too much inflammation can occur. Hives are one example of a stress-induced breakdown in the Immune System’s patrols.”
- (Ref 7) Exercise; Meditate; Have a hobby; Talk to a trusted friend; Practice regular and conscious breathing throughout the day and when feelings of stress arise.
- (Ref3, Ref 7) “Stress releases hormones like cortisol that suppresses inflammation (inflammation is initially needed to activate immune cells) and the action of White Blood Cells.”
Keep Your Vaccinations Up To Date
Ref 4; Ref 5; Ref 6; Ref 10; Ref 11
- (Ref 4) “Vaccines, also called immunizations, teach the Immune System to make antibodies that fight off infections before they make you sick.”
- (Ref 11) Keep your vaccinations up to date. “Vaccines introduce your Immune System to viruses in a very controlled manner”. This becomes more critical as you age and your Immune System weakens.
It’s Difficult to “Prove” Many of the Suggested Benefits
Ref 3; Reg 5; Ref 12; Ref 14)
Due to the complicated and interconnected nature of our body systems, it’s very difficult to scientifically prove many of the stated Immune System benefits.
- (Ref 3) “…there’s no magic “healthy pill””
- (Ref 5) “For now, there are no scientifically proven direct links between lifestyle and enhanced immune function.”
- (Ref 12) “I think a misconception is that there are supplements or products out there that can really boost the Immune System. Unfortunately, they haven’t really had robust evidence that they’re highly effective,..”
- (Ref 14) “There is no strong evidence to prove that taking immune supplements along with exercising lowers the chance of illness or infections.”
That doesn’t mean you can’t find a reasonable approach to improving your overall health and assuming that your immune health will benefit also.
References for Immune System Improvement Advice
- CDC – Healthy Habits: Enhancing Immunity
- Clevelendclinic.com – 5 Vitamins That Are Best for Boosting Your Immunity
- Clevelandclinic.com – Strengthen Your Immune System With 4 Simple Strategies
- Columbia.edu – what-you-really-need-do-boost-your-immunity
- Harvard.edu – How to boost your Immune System
- Harvard.edu – Immune boosts or busts? From IV drips and detoxes to superfoods
- Harvard.edu – Nutrition and Immunity
- Harvard.edu – Some Benefits of Exercise Stem from the Immune System
- Harvard.edu – What can you do to improve your Immune System?
- HHS.gov – Vaccines Protect You
- Mayoclinic.org – Aging and the Immune System
- Mayoclinic.org- How to maintain a healthy Immune System
- Mayoclinic.org – Lack of sleep: Can it make you sick?
- Medlineplus.gov – Exercise and Immunity
- NIH.gov – Dietary Supplements for Immune Function and Infectious Diseases
Conclusion
Your body’s Immune System is an amazing collection of organs, cells, and chemicals that possess an “armada” of both innate (born with) and adaptive (specific and possessing memory) “weapons” to combat pathogens and other harmful “agents” (e.g. cancerous cells, wounds, toxins, etc.).
At birth we are already protected with various physical (skin, mucous membranes ) and chemical barriers (pH, heat, microbes) that keep harmful agents out of our bodies.
We also possess White Blood Cells that at birth can digest or otherwise destroy harmful agents (e.g. Phagocytes and Natural Killer Cells.).
One of the most amazing aspects of our Immune System is its ability to not only target and destroy specific pathogens (and other bad actors) but also to provide immunity by retaining White Blood Cells specially designed to destroy them in the future (B-Cells and T-Cells). We call this our Adaptive Immune System.
Our Adaptive Immune System allows us to vaccinate against disease and illness.
Vaccinations introduce mild doses of specific pathogens into our bodies. This allows B and T White Blood Cells (and Antibodies) to specialize in the present and future destruction of these bad actors (thus providing immunity).
Two last things:
- Be amazed and
- nurture and take of this amazing and complicated system by regularly exercising and eating properly.
Appendix 1 – Blood Components
The tree chart below shows the various blood components derived from Hematopoietic Stem Cells.
Hematopoiesis (from Greek ‘blood’ and ‘to make’) is the formation of blood cellular components from Stem Cells. We specify the Stem Cells involved in this as hematopoietic since other types of Stem Cells exist.
Hematopoietic Stem Cells reside (mostly) in bone marrow. So your bones are not just your body’s structural support system, it’s also the body’s blood cell factory!!
According to the Icahn School of Medicine , “Cells that circulate in your blood include immune cells (White Blood Cells), Red Blood Cells, and Platelets. Your body produces an astonishing 100 billion blood cells each day.”
Chart_Blood Components Derived from Hematopoietic Stem Cells
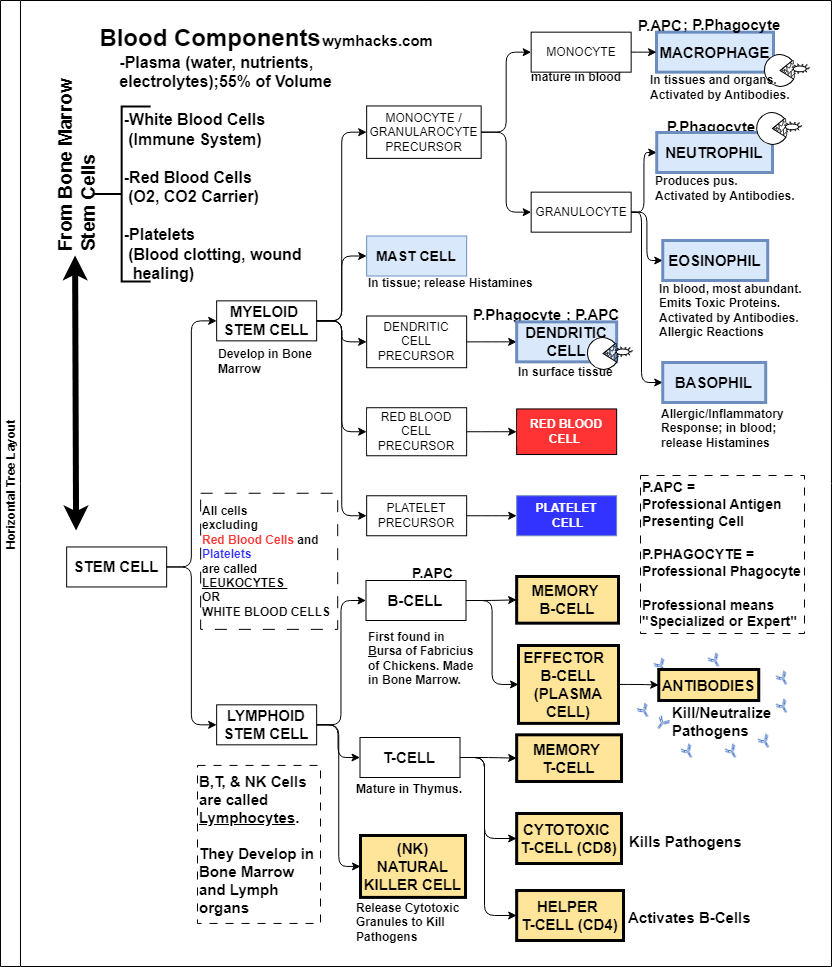
According to the my.clevelandclinic.org, blood by volume is about 45% Red Blood Cells, 55% Plasma, and 1% White Blood Cells + Platelets.
Chart_Blood Composition by Volume
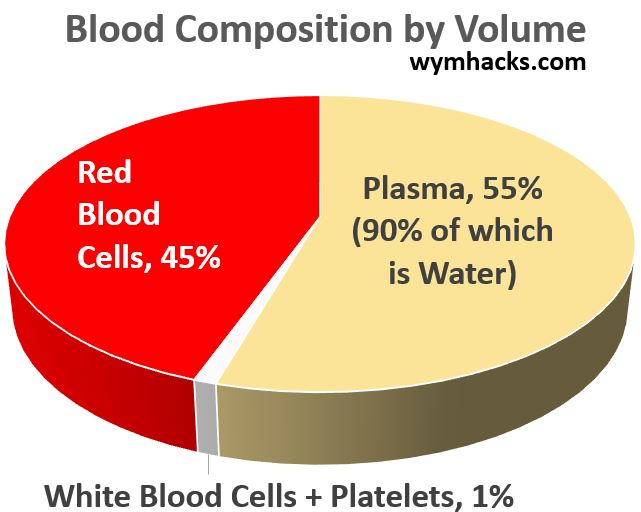
We’ll focus on the Non-Plasma components of blood and especially the White Blood Cells (WBCs).
Hematopoietic Stem Cells mostly residing in bone marrow, are the progenitors of all Red Blood Cells, Platelets, and White Blood Cells (WBCs).
White Blood Cells are also called Leukocytes.
Myeloid Stem Cell Derived White Blood Cells
The chart below is a zoom in on the Myeloid Stem Cell section of the full chart shown above.
Chart_Blood Cell components from Myeloid Stem Cells
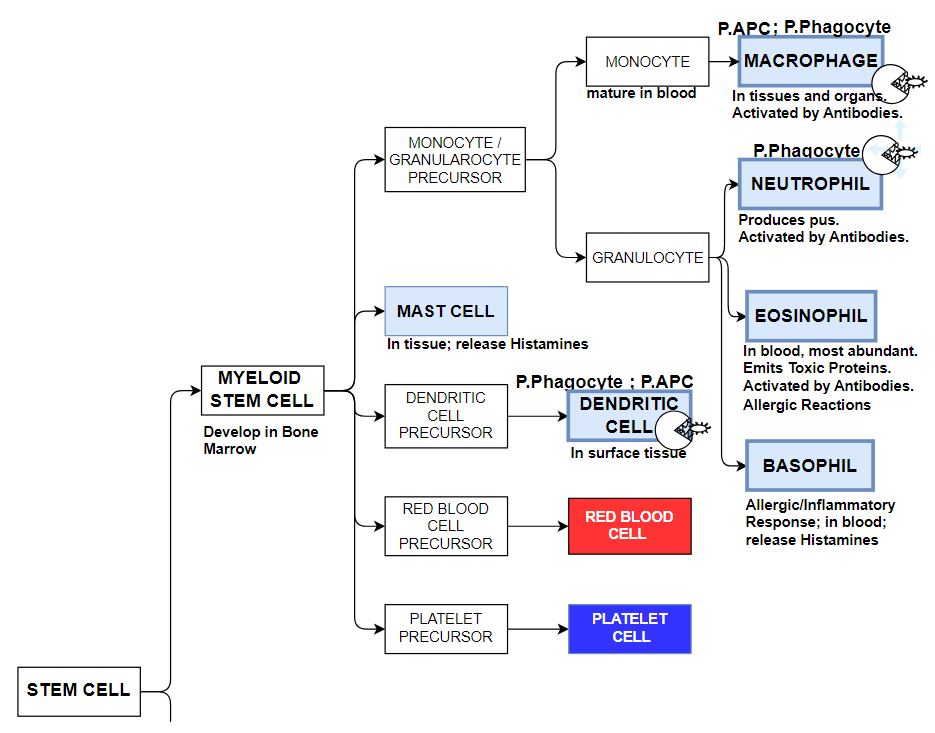
Myeloid Stem Cells are the progenitors of Red Blood Cells and Platelets as well as several White Blood Cell (WBC) types.
Myeloid Stem Cell derived White Blood Characteristics
- Play a role in the Innate Immune Response system as well as the Adaptive System
- They have different weapons and tools to combat pathogens.
- Phagocytes (see the PAC MAN figures in the chart), engulf and essentially dissolve the pathogen.
- Others use chemicals as weapons against pathogens or create allergic responses.
- Some present Antigens on their surfaces to be utilized in the Adaptive Immune Response system
- Professional (i.e. specifically equipped) Phagocytes :
- Different references are inconsistent in identifying Professional Phagocytes.
- Neutrophils: (most abundant White Blood Cells; first responders)
- Macrophages
- Dendritic Cells
- Mast Cells: (some sources identify these as Professional and others don’t)
- Professional Antigen Presenting Cells (P.APC)
- Macrophages and Dendritic Cells are Professional Antigen Presenting Cells.
- They Engulf the pathogen, Break it up into bits, Reject them, but also present some bits (peptide chains) on the surface (called an Antigen).
- Antigen is short for Antibody Generator.
- Antigens help activate Adaptive Response White Blood Cells (more later).
Lymphoid Stem Cell Derived White Blood Cells
The chart below is a zoom in on the Lymphoid Stem Cell section of the full chart shown above.
Chart_Blood Cell components from Lymphoid Stem Cells
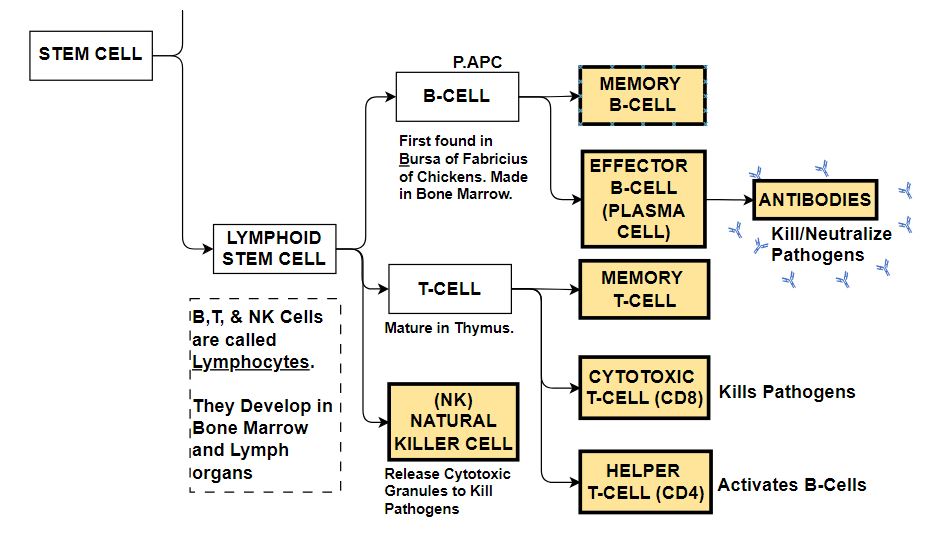
Lymphoid Stem Cells produce three types of Lymphocytes: Natural Killer Cells, B-Cells and T-Cells.
Natural Killer Cells play both an innate response role and an adaptive response role while B-Cells and T-Cells are the major Adaptive Immune Response System players.
Natural Killer (NK) Cells
- Can non-specifically sense and destroy pathogens by releasing cytotoxic Granules (Part of Innate Response)
- Can interact with Antibodies to target and destroy specific pathogens (Part of Adaptive Response)
B-Cells
- Discovered in the Bursa of Fabricius of Chickens
- They are made (and also mature) in bone marrow.
- B-Cells are part of the body’s Adaptive Immune Response,
- Involved in extracellular defenses (Humoral Response)
- Attaching to a pathogen partially actives it.
- B-Cells can engulf pathogens and present their Antigens on their surface.
- This Antigen Presenting capability allows T-Cells to activate them.
- A fully activated B-Cells will produce Memory Cells and Effector Cells (Plasma Cells).
- Plasma Cells release Antibodies into the blood stream to combat pathogens.
T-Cells
- Made in bone marrow and mature and develop in the Thymus.
- T-Cells are part of the body’s Adaptive Immune Response.
- Involved in both extracellular (Humoral Response) and intracellular defenses (Cell Mediated Response)
- T-Helper (CD4) Cells interact with Antigens on B-Cells to activate B-cells. They also activate T-Cytotoxic cells.
- T- Cytotoxic (CD8) Cells release chemicals that kill pathogens that have infiltrated cells (e.g. cancer cells or cells infected with virus).
What Do These Cells Look Like?
Apart from Red Blood Cells, White Blood Cells will have a white or transparent color. Various colored dyes are used to identify them.
The picture below shows my renditions based on various web based sources. The cells are generally and very roughly described by the following characteristics:
- overall roundness
- size of nucleus
- shape of nucleus
- presence of granules and other bodies inside them
- relative size
Picture – Stem Cell Derivatives
Disclaimer: The content of this article is intended for general informational and recreational purposes only and is not a substitute for professional “advice”. We are not responsible for your decisions and actions. Refer to our Disclaimer Page.